BMJ Best Practice: Your Evidence Based Clinical Companion Anytime Anywhere
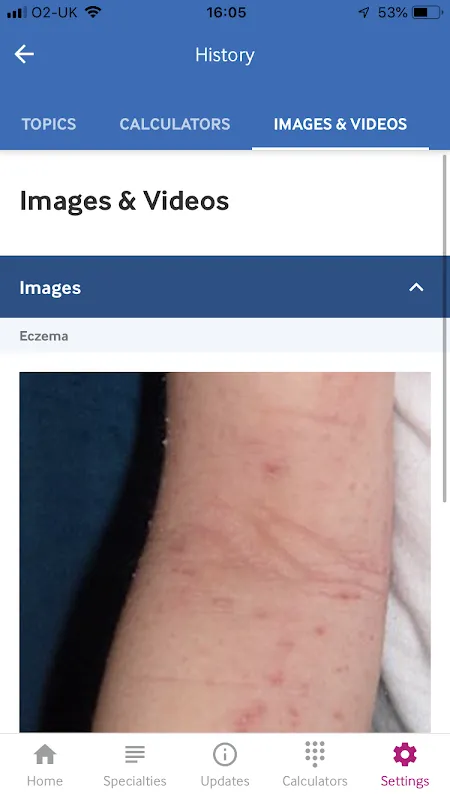
Staring at that puzzling rash at 3 AM with no senior colleagues around, my palms grew damp until I remembered the trial icon on my tablet. That first tap felt like floodlights switching on in a dark theater – suddenly every differential diagnosis lay clearly mapped with treatment pathways. This isn't just another medical reference; it's the clinical partner I now reflexively reach for during those breathless moments between patient rooms.
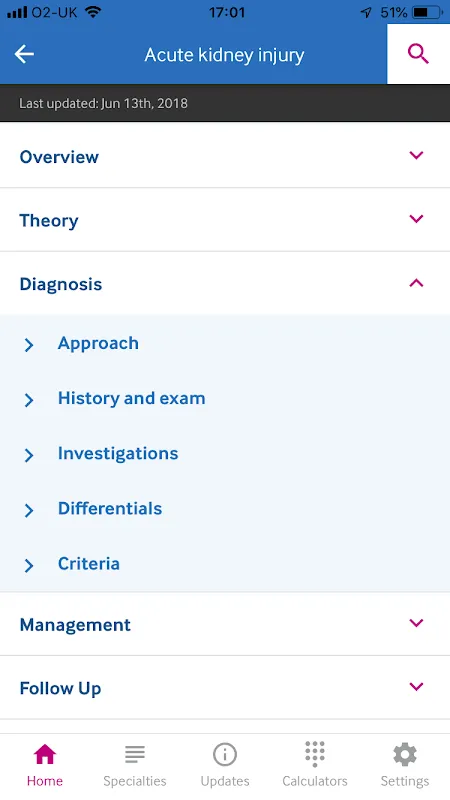
Instant Evidence Based Guidance became my anchor during complex rounds. When Mrs. Henderson presented with overlapping autoimmune symptoms last Tuesday, the app's layered decision trees transformed my initial confusion into structured action within minutes. That tangible shift from uncertainty to clinical confidence still sends relief through my shoulders whenever I open a new case file.
Patient Education Leaflets turned awkward conversations into bonding moments. Watching Mr. Peterson's eyes lose their fear as we scrolled through the visual medication guide together – his finger tracing the animated dosage timeline – created more understanding than my hurried explanations ever did. Now I preload these before consultations, watching anxiety dissolve as patients hold tangible answers in their hands.
Integrated Medical Calculators saved me during a code blue last month. With adrenaline making mental math impossible, the heparin calculator gave precise dosing while my trembling hands stabilized the IV line. That cold ER tile against my knees as the numbers flashed up? That's when I stopped seeing tools and started seeing a lifeline.
Procedure Demonstration Videos transformed my fellowship jitters into competence. Preparing for my first lumbar puncture, I replayed the oblique needle angle sequence six times on night shift, fingers unconsciously mimicking the motion against empty air. Next morning, the tactile memory guided my hands smoother than any textbook diagram ever could.
Offline Clinical Library proved invaluable when our hospital Wi-Fi crashed during hurricane alerts. As generators hummed in the background, I downloaded emergency protocols for twelve critical patients with one trembling thumb swipe. That blue glow illuminating treatment paths while rain lashed the windows? That's technological reliability redefined.
Monday 7:45 PM finds me reviewing CME credits while my coffee cools untouched. The app's automatic tracking feature quietly tallied my journal reading into certification hours last quarter – no more frantic spreadsheet nights before renewal deadlines. Those green progress bars now feel like silent colleagues nudging me toward growth.
Wednesday 3:00 AM in the call room: moonlight stripes the wall as I toggle night mode. The screen's warm amber glow lets me check sepsis protocols without searing my retinas before returning to the wards. This thoughtful design detail matters more than developers might realize during our bleary-eyed vigils.
Yes, I wish medication interaction alerts were more prominent during prescription workflows. And that one time the cardiology calculator loaded slower than my pounding heart during an MI case? We all have improvement wishes. But when Dr. Reynolds asked about alternatives yesterday, my answer came instantly: Try the seven-day trial during your next ICU rotation. See how evidence-based clarity feels when minutes matter.
Keywords: BMJ Best Practice, clinical decision support, medical reference, healthcare app, evidence based medicine