Eyedea Refractive: The Essential Surgical Calculator for Precision LASIK/PRK Outcomes
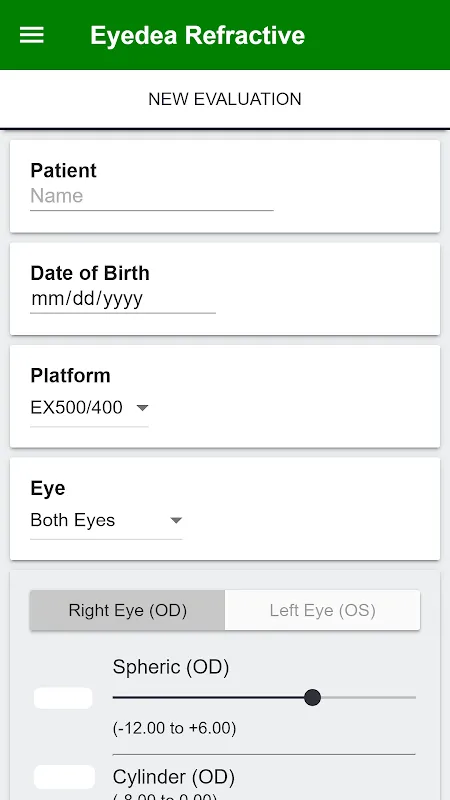
Staring at the flickering spreadsheet at 2 AM, my coffee cold beside surgical plans, I felt that familiar knot of anxiety - one decimal miscalculation could alter a patient's vision forever. Then I discovered Eyedea Refractive during a desperate search. From the first calculation, its clinical precision dissolved my doubts like morning fog. Created specifically for refractive surgeons, this isn't just another app; it's the digital assistant that finally lets surgeons breathe easy during pre-op evaluations.
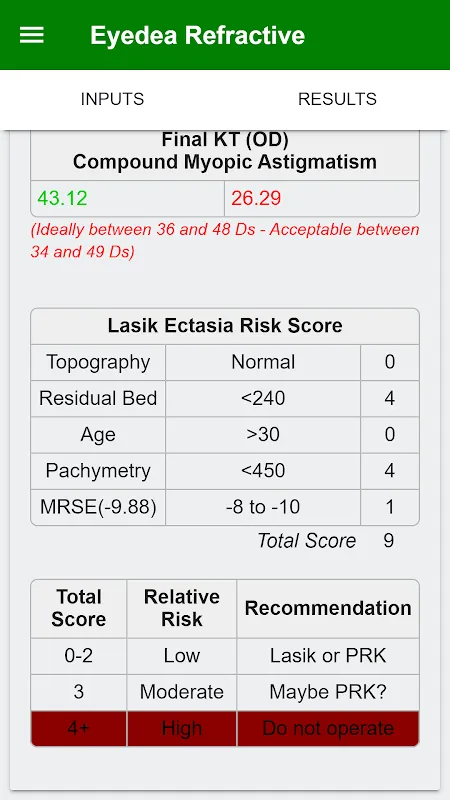
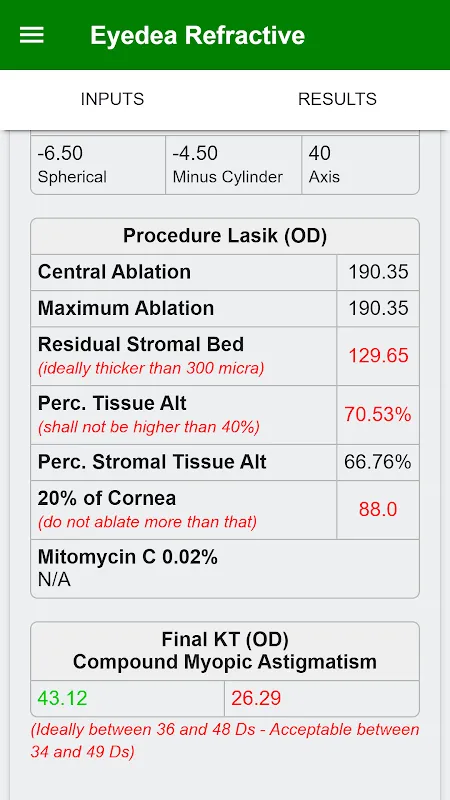
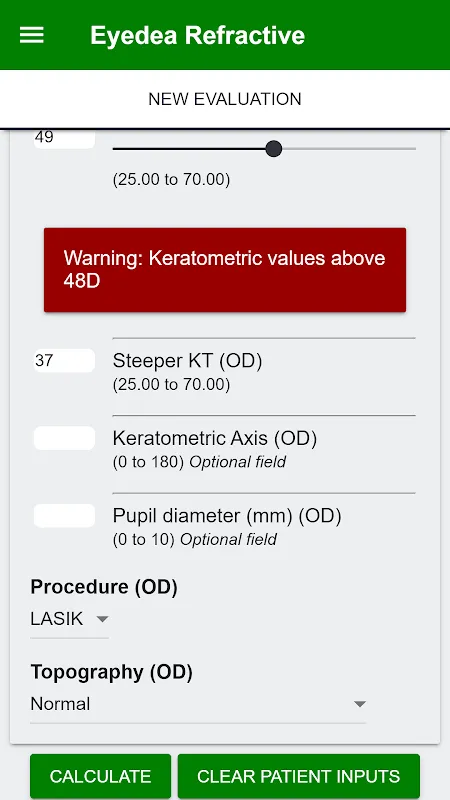
Flap Parameter Intelligence transformed my planning routine. Inputting intended flap thickness and optical zone dimensions while prepping for Friday surgeries, I watched the interface instantly generate ablation depth projections. That moment when residual stromal bed calculations first appeared - green safety margins glowing against clinical thresholds - felt like surgical headlights cutting through darkness. Now I cross-verify every case, fingertips tracing the safety buffer between success and complication.
Nomogram Refraction Engine became my secret weapon for unpredictable corneas. Last Tuesday, preparing for a post-RK patient, I entered irregular topography readings. When the adjusted refraction blinked onto the screen - differing 0.75D from my manual estimate - I actually laughed aloud in the empty clinic. Three weeks post-op, that patient achieved 20/15 vision. The algorithm's foresight now feels like having a veteran colleague whispering over my shoulder.
Mitomycin C Timer turns tense moments into rhythmic precision. During a PRK enhancement last month, haze threatened at the peripheral zone. As the app's countdown pulsed softly from my tablet, the calculated 23-second exposure time became my metronome. Swabbing the sponge in perfect sync with the vibration alert, I realized this feature had eliminated my old stopwatch fumbles. That chemical tang in the OR air now carries confidence instead of stress.
Mid-morning consultations transformed with LERS Predictions. Young athletes squinting at my light refraction charts would tense until I showed Eyedea's laser energy distribution simulations. Watching their shoulders relax as colored heat maps demonstrated safety margins - that visual trust-building is priceless. Yesterday's college pitcher even photographed his PSTA results to show nervous parents.
Tuesday dawns find me in surgical blues, morning light glinting off the autoclave as I input final parameters. The instant ablation depth confirmation - displayed beside the patient's name - always triggers that last deep breath before scrubbing in. Post-op at sunset, reviewing final KT readings against projections with jazz playing softly, each aligned decimal point feels like a standing ovation.
The brilliance? It launches faster than my slit lamp powers up - critical when urgent calculations interrupt surgery prep. Seeing PTA percentages update live while adjusting laser settings delivers tangible relief. But I wish the stromal bed visualization allowed manual contour adjustments for irregular corneas; during that severe keratoconus case last quarter, I craved finer control. Still, watching residents input their first calculations - those widened eyes when nomogram adjustments materialize - confirms this is indispensable.
For ophthalmologists transitioning from manual calculations to laser precision, this isn't just helpful - it's practice-transforming. Perfect for surgeons needing that second pair of digital eyes during critical pre-op decisions.
Keywords: refractive surgery, Lasik, PRK, nomogram, stromal bed