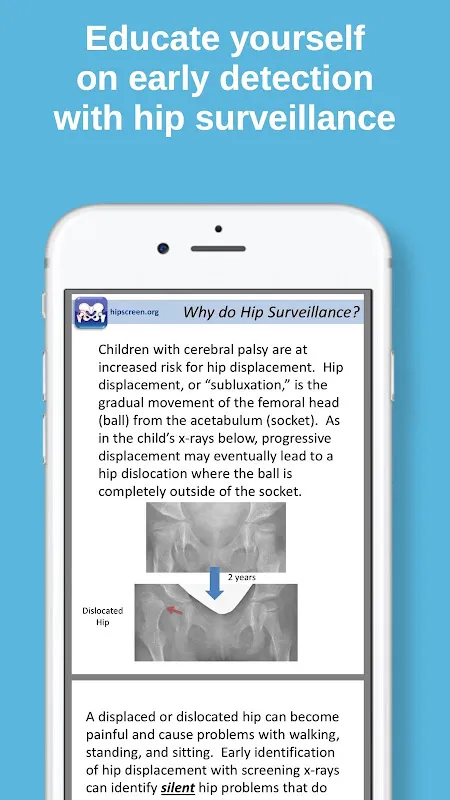
As a pediatric physical therapist with over a decade in neuromuscular clinics, I've witnessed too many children with cerebral palsy lose mobility to preventable hip complications. That sinking feeling when reviewing late-stage X-rays – seeing joints beyond salvage – haunted me until discovering HipScreen. This app fundamentally transformed my approach, turning reactive despair into proactive hope through its meticulously designed early detection system.
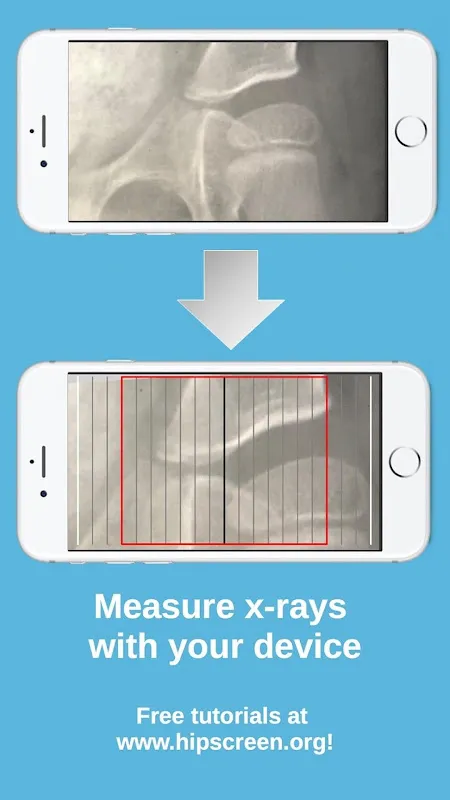
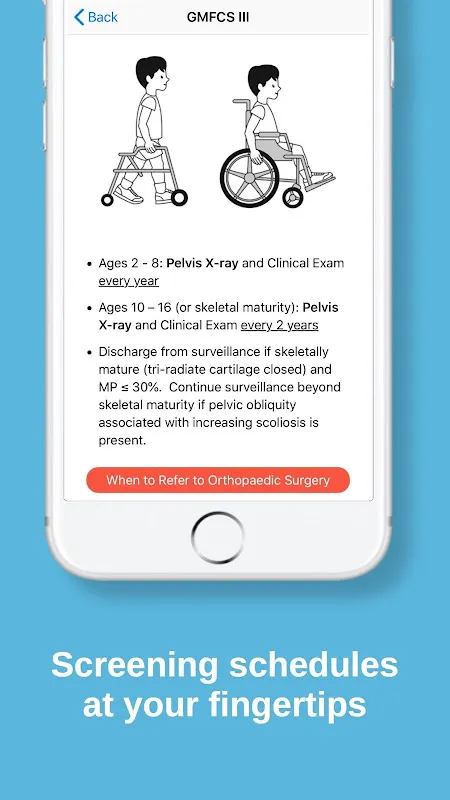
The educational modules felt like attending a global CP symposium from my clinic sofa. When preparing for a complex case last Tuesday, the peer-reviewed literature section illuminated subtle risk factors I'd previously overlooked. That moment of realization – fingers freezing mid-scroll as research connected clinical dots – gave me confidence to advocate for earlier imaging. The protocols section became my daily compass, particularly when training new staff. I recall guiding a flustered technician through perfect X-ray positioning using the visual guides; her relieved exhale when capturing the ideal lateral view mirrored my own first experience. The measurement tools revolutionized my workflow during hectic morning rounds. Last month, while analyzing migration percentages for twin patients, the instant calculation feature spotted asymmetries my fatigued eyes missed. That subtle vibration alert felt like a colleague tapping my shoulder with life-changing news.
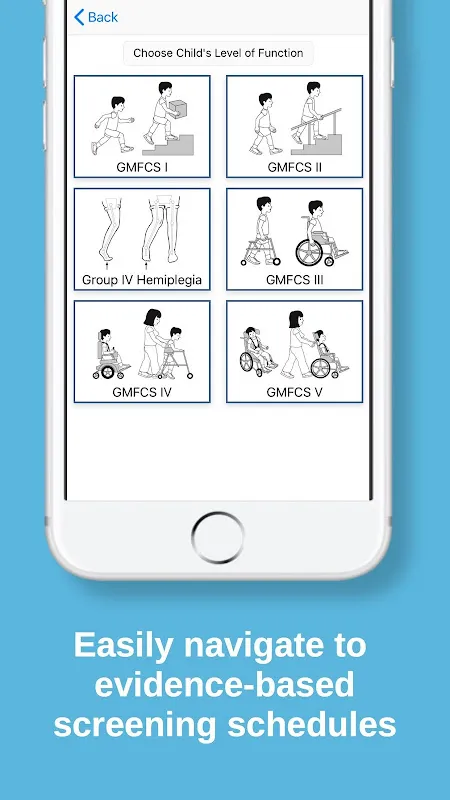
Picture this rainy Thursday afternoon: fluorescent lights humming in our treatment room as I position a nonverbal seven-year-old for assessment. With HipScreen open on my tablet, I reference surveillance timelines while parents watch anxiously. The app's clear graphics transform medical jargon into visual stories – I see shoulders relax as families finally understand why we recommend biannual imaging. Later, during interdisciplinary meetings, I project comparative measurements showing slowed disease progression since implementing their guidelines. That collective nod from surgeons and physiatrists validates what data already confirmed.
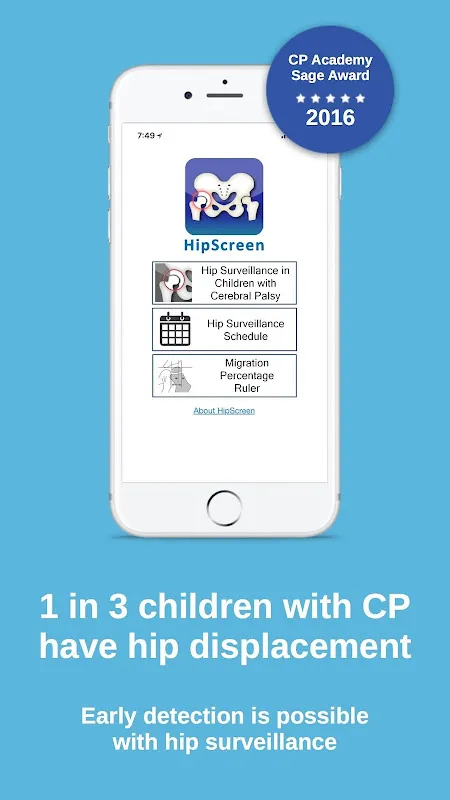
What makes HipScreen indispensable? It launches faster than emergency protocols during critical consultations. The interface remains intuitive even after midnight charting sessions when coffee wears thin. Yet I wish for customizable alert thresholds – during a recent ski trip, urgent notifications about a patient's rapid migration percentage got buried under resort emails. While the AACPDM award speaks volumes, true validation comes from children like my patient Sofia. Two years into surveillance, we caught subluxation at 28% displacement. Post-surgery, she now practices walking frames with pain-free determination – living proof that early detection preserves futures.
For therapists drowning in complex caseloads or rural doctors lacking specialist access, this app bridges critical gaps. Though not a diagnostic replacement, it's the vigilant partner we need in the relentless pursuit of preserving young mobility.
Keywords: cerebral palsy early detection, hip displacement prevention, pediatric mobility preservation, radiographic surveillance protocols, clinical measurement tools