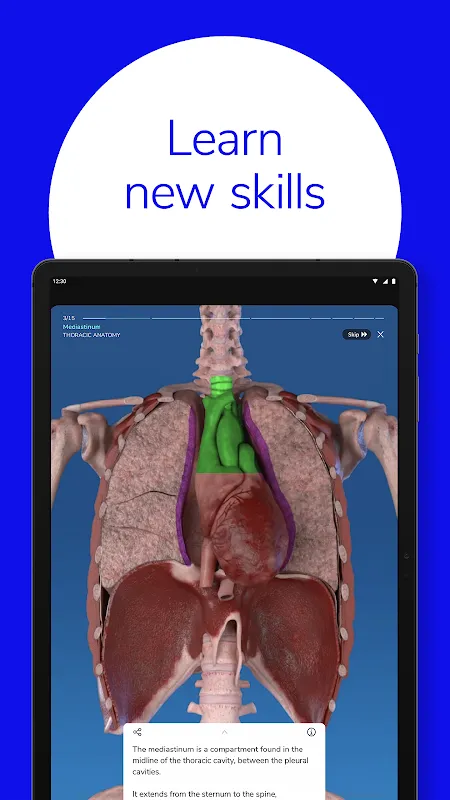
Touch Surgery App: Lifelike 3D Surgical Training Anytime, Anywhere
During my third-year neurosurgery rotation, I froze when the attending asked me to demonstrate a craniotomy approach. Textbook diagrams felt flat, and cadaver labs were scarce. That's when a senior resident showed me Touch Surgery. From that panicked moment, this app became my digital mentor – transforming subway commutes and call room downtime into immersive OR rehearsals. Designed for surgeons, residents, and healthcare professionals, it bridges the gap between theory and muscle memory with astonishing realism.
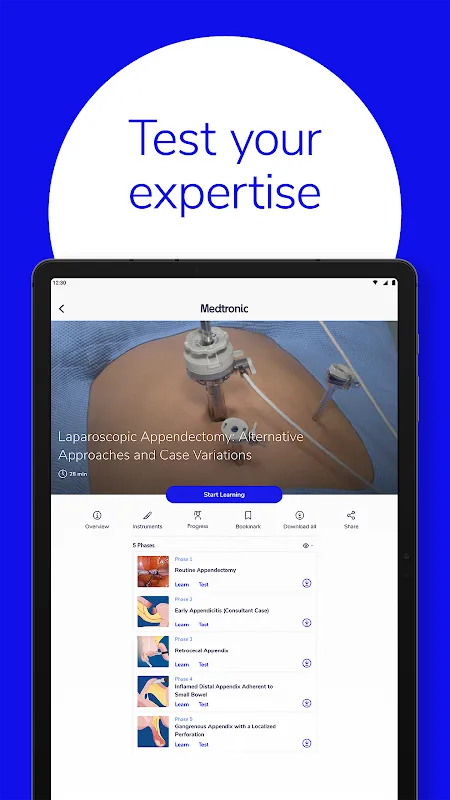
Step-by-Step Surgical Simulations became my pre-op ritual. Before my first solo tendon repair, I repeated the virtual procedure 17 times on my tablet. The tactile feedback when "suturing" digital tissue created surprising muscle memory. During the actual surgery, my hands recalled the motion sequence instinctively – that moment of realization still gives me chills.
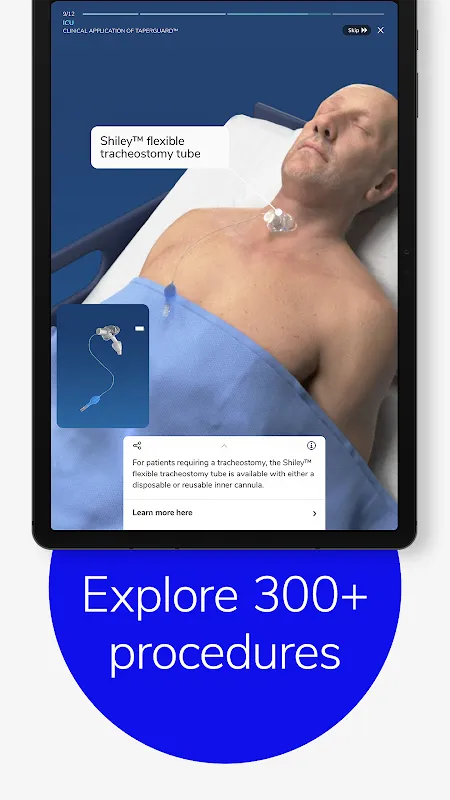
Massive Specialty Library saved me during a rural rotation. When an emergency hand trauma case arrived, I quickly pulled up the flexor tendon module during the helicopter ride. The immediate access to rare procedures feels like having a surgical encyclopedia that fits in your scrub pocket. I've discovered unexpected cross-specialty applications too – ophthalmology techniques that improved my microvascular skills.
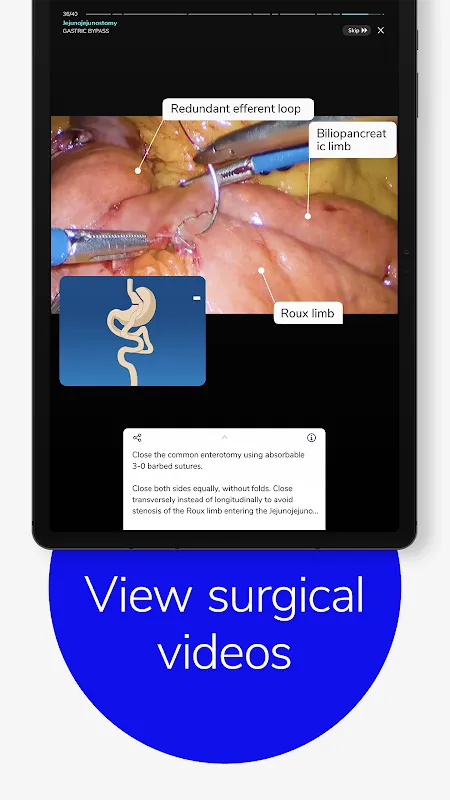
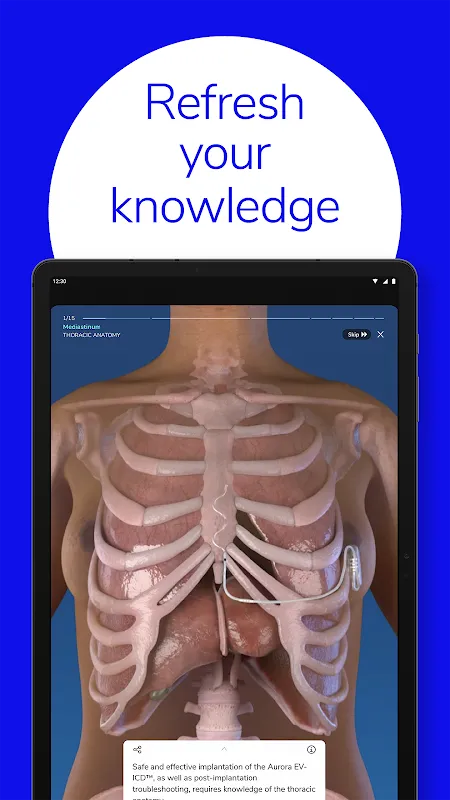
Cinematic 3D Graphics redefine spatial learning. Rotating a virtual fractured femur at 2 AM, I noticed trabecular patterns I'd missed in textbooks. The lighting on tissues changes as you adjust angles, revealing anatomical relationships like physical specimens. When I first saw blood vessels pulsate in a simulation, my brain registered it as a real physiological response.
Master Surgeon Demonstrations offer priceless mentorship. Watching a world-renowned vascular surgeon narrate aneurysm clipping techniques, I noticed subtle instrument rotations never mentioned in literature. Their commentary anticipates common pitfalls – "Notice how I avoid this nerve bundle" – creating apprenticeship moments during night shifts.
Free Core Curriculum with specialty upgrades respects career progression. As an intern, the free orthopedic modules built my foundation. Now as a fellow, purchasing the advanced neurosurgery pack felt like investing in custom-tailored education. The pricing structure recognizes that surgical mastery evolves over decades.
Tuesday 3:17 AM in the call room: Monitor glow illuminates my face as I rehearse emergency burr holes. Haptic feedback vibrates through the stylus with each "bone drill" pass. The virtual drill sound syncs perfectly with tactile resistance – a multisensory experience that made my first real cranial decompression feel familiar.
Saturday airport terminal: Between flights to a conference, I complete a virtual rhinoplasty using my phone. Travelers glance curiously as my fingers manipulate invisible instruments. For 28 minutes, gate B12 becomes an OR where I can safely experiment with graft techniques impossible to practice on live patients.
What works brilliantly? The procedural accuracy – my attending spotted improved trocar placement after just two weeks of virtual practice. The community aspect too; discussing simulation metrics with colleagues creates objective skill benchmarks.
What needs refinement? Heavy 3D rendering drains batteries during marathon sessions. I now carry backup power banks. More ENT modules would balance the current orthopedics-heavy library.
For surgical residents drowning in theory but starved for hands-on time, this app is oxygen. It won't replace the feel of real tissue, but it builds the neural pathways that make your first incision feel like your hundredth.
Keywords: surgical simulation, 3D medical training, surgical education, residency preparation, procedural rehearsal