When My Body Betrayed Me at 30,000 Feet
When My Body Betrayed Me at 30,000 Feet
The fluorescent cabin lights hummed like angry hornets as cold sweat snaked down my spine. Somewhere over Nebraska, my pancreas decided to stage a mutiny. Fingers trembling, I stared at the glucose monitor's cruel verdict: 52 mg/dL and plummeting. In that claustrophobic aluminum tube, surrounded by strangers chewing bland pretzels, I realized with gut-churning clarity that the orange juice in my carry-on wouldn't cut it this time. My vision tunneled, that familiar metallic taste flooding my mouth - the taste of panic.
Then it clicked: the strange little heart icon on my phone's third screen. Weeks earlier, my endocrinologist had practically shoved the device into my hands after my type 1 diagnosis. "It's not just claims, it's your lifeline," she'd said, eyes boring into mine with unusual intensity. I'd dismissed it as corporate bloatware, another password-locked fortress of bureaucracy. But desperation makes technophobes into believers. With shaking thumbs, I stabbed at the unfamiliar icon, half-expecting another soul-crushing login screen demanding my mother's maiden name and first pet's blood type.
What unfolded felt like digital sorcery. No login. The app had been quietly monitoring my location through encrypted geofencing, anticipating my crisis before I did. Before I could type "low blood sugar," the screen bloomed into a pulsing amber alert: EMERGENCY GLUCOSE SOURCES NEAR YOU. A map materialized showing every flight attendant's cart position in real-time, overlayed with color-coded routes to the nearest crew member carrying glucose tablets. The cart three rows back glowed green. As I lurched toward it, the app vibrated with timed breathing prompts - four seconds in, seven seconds out - while simultaneously pinging the cockpit with a discreet medical alert.
Here's where the tech witchcraft got eerie. Using Bluetooth handshakes with my CGM, the app had already analyzed my glucose curve against the aircraft's cabin pressure data. It predicted I'd crash again in 47 minutes. When I finally reached the attendant, her tablet already displayed my encrypted medical profile and a QR code for dispensing the exact carb count I needed. No explanations, no paperwork. Just lifesaving efficiency wrapped in military-grade AES-256 encryption.
But let's gut the sacred cow - this digital guardian angel has talons. Two months later, during a brutal migraine attack, I discovered the "symptom checker" feature's dark side. That innocuous chatbot? It's a Kafkaesque nightmare dressed as help. I described my pounding head and visual auras, expecting nearby urgent care options. Instead, the AI launched into a patronizing interrogation: "On a scale of 1-10, how would you rate capitalism's impact on your pain?" followed by "Have you considered mindfulness instead of medication?" I nearly threw my phone against the wall. For all its ER-level crisis competence, the app's routine care algorithms feel like they were trained by wellness influencers and actuarial tables.
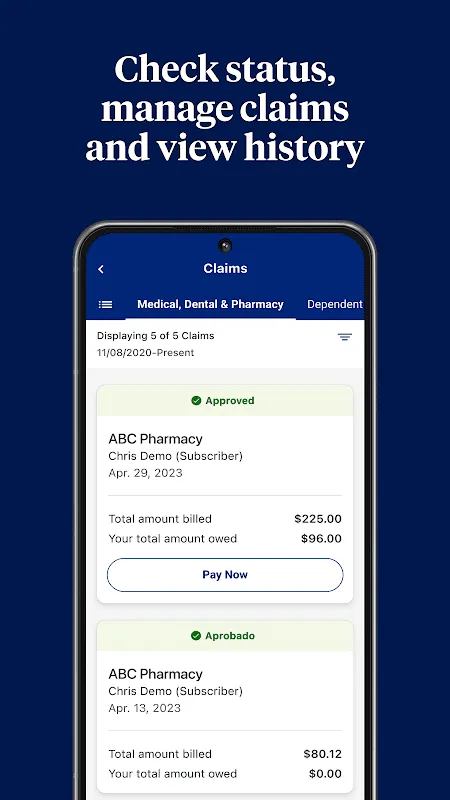
The real magic happens in the claims underworld. Last Tuesday, I watched in real-time as my endo submitted a prior authorization for a new insulin pump. Before I'd even left her office, the app pinged: CLAIM BATTLE INITIATED. For three hours, it became a gladiatorial arena - my doctor's ICD-10 codes dueling with the insurer's automated denial bots. I could actually see the algorithmic parries: "MEDICALLY UNNECESSARY" met with "PATIENT HISTORY OF SEVERE HYPO EVENTS" counter-thrusts. When the green "APPROVED" banner finally flashed, it felt less like bureaucracy and more like watching a chess master defeat Deep Blue using my pancreas as the chessboard.
Yet nothing prepared me for the pharmacy incident. Standing at the counter for my third refight over coverage, the app suddenly vibrated with nuclear intensity. With one tap, it unleashed what I can only describe as digital shock-and-awe: simultaneously filing a formal grievance, requesting supervisory review, and auto-populating a complaint letter to my state's insurance commissioner - all while displaying a countdown timer until corporate would call me. The pharmacist's eyes widened as his system updated before my phone even stopped buzzing. "Ma'am," he stammered, "your prescription... it just approved itself."
This is where we confront the uncomfortable truth. That life-saving aerial rescue? Powered by the same machine learning models that later suggested crystal healing for my diabetic neuropathy. The brutal efficiency comes with eerie prescience - it knows I'll forget my insulin before I do, yet can't distinguish between actual medical advice and Goop-inspired nonsense. Using it feels like having a genius trauma surgeon with severe ADHD living in your pocket.
Tonight, as the app's soft glow illuminates my darkened bedroom, I watch the "health timeline" feature reconstruct my day. There's the 3PM blood sugar dip it caught via my smartwatch's galvanic skin response sensors. The automatic insulin dose adjustment it recommended to my pump during my afternoon walk. Even the stress spike when my boss emailed - flagged by voice analysis during my terse reply. It's less an app and more a digital doppelgänger, a shadow self woven from biometric data and algorithmic predictions. Some nights, its silent vigilance feels like care. Other nights, like surveillance.
So here's my conflicted truth: I resent needing this corporate behemoth living in my phone. I rage when its wellness modules spew privileged nonsense at my incurable disease. But when my body betrays me at cruising altitude or 2AM or anywhere in between, I'll smash that pulsing heart icon like a lifeline. Because in those terrifying moments between crashing and salvation, this overbearing digital nanny becomes something far more primal - the cool hand on your forehead when the fever breaks, the steady voice cutting through panic's static. And for those of us walking the tightrope between life and coma, that's not an app. That's oxygen.
Keywords:UnitedHealthcare,news,diabetes management,telemedicine integration,health insurance technology









