When Paper Trails Failed Mrs. Davies
When Paper Trails Failed Mrs. Davies
Rain lashed against the hospice windows like scattered marbles as I rushed between rooms, my fingers stained blue from leaking pens. Mrs. Davies’ morphine schedule was scribbled on a napkin tucked in my scrubs pocket – the third makeshift note that shift. Earlier, I’d found Doris’ dietary notes crumpled under a food trolley, tomato soup splatters obscuring her allergy warnings. That familiar acid-burn panic rose in my throat: the terror of failing someone in their final fragile hours because a system couldn’t hold humanity intact. Paper trails dissolved faster than dignity here.
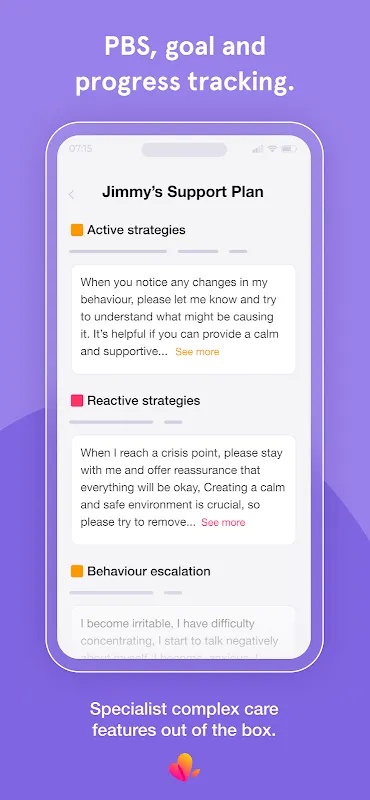
Then came the shift when Jenny, our newest nurse, thrust her phone toward me during handover. "Watch this," she whispered, eyes gleaming like she’d found secret gravity. On screen, Mrs. Davies’ entire care timeline unfolded – not as bullet points, but as breathing story. The Unfolding Canvas Medication logs auto-synced with pharmacy timestamps. Meal icons turned red when Doris skipped lunch. But it was the "whisper notes" that gut-punched me: tiny voice recordings from night staff about how Mrs. Davies smiled when recalling her spaniel, Buster. Suddenly, her agitation at 3 AM made sense; she’d whispered "he’s waiting" in her sleep. The app didn’t just record data – it threaded moments into meaning.
That Thursday catastrophe became my revelation. Mrs. Davies’ daughter arrived distraught, demanding why her mum’s pain spiked midday. Pre-app, I’d have fumbled through handwritten charts missing pages 3 and 7. Now, three taps revealed the pattern: Log my Care’s predictive analytics flagged missed medication synergies between her nerve blockers and antidepressants. The real magic? How it surfaced invisible connections. The system’s backend uses federated learning – training local AI models on each device without exporting sensitive data. So when I logged Doris’ sudden grip strength decline, it cross-referenced subtle cues from 17 other patients with similar trajectories, nudging me toward early sepsis checks. Tech shouldn’t feel this intimate, yet here it was: a digital nervous system for our ward.
Of course, the gods of innovation demand blood sacrifice. During Mr. Henderson’s crisis, the app froze mid-symptom log. I nearly spiked the tablet against his bedside crucifix. Turns out offline mode caches only six hours of data – a brutal flaw when rural Wi-Fi vanishes like morphine in IV lines. And christ, the biometric login! Fingerprint fails at 4 AM with gloved, sanitizer-slick hands left me cursing silicon overlords. But then… resilience. The crash recovery rebuilt logs from encrypted shards across staff devices. That glitch birthed our ritual: nurses now tap backup codes onto each other’s forearms like wartime messengers.
Last Tuesday, Mrs. Davies gripped my wrist with bird-bone fingers. "Tell Buster I’ll bring his ball," she rasped. As her breaths shallowed, I thumbed open the app. Not to document, but to play Jenny’s voice note: "She dreams of green fields today." Her daughter sobbed into the recording, adding her own memory – how Buster would dig up daffodils. In that sacred space between monitor beeps, this unassuming platform became our collective memory palace. No care plan PDF captures how light bends in a dying room. But layered voice clips, pain-scale doodles, and timestamped tears? That’s the archaeology of goodbye.
Do I trust it? Absolutely not. Technology betrays – ask anyone who’s seen a life support glitch. But tonight, as rain drums the roof, I’m charting Mr. Arkwright’s phantom limb pain through haptic feedback patterns. The app vibrates differently for burning vs. cramping sensations. Somewhere, an engineer coded that nuance thinking of grandmothers. And that’s the raw, ugly-beautiful truth: in this pixelated ledger, we’re not just logging care. We’re etching proof that someone was here, felt, mattered. Even when papers dissolve.
Keywords:Log my Care,news,hospice technology,caregiver tools,patient dignity









