My hands trembled over the ventilator controls as alarms screamed through the trauma bay. Another crashing patient, electrolytes in chaos, and no time for textbook flipping. That sinking feeling of seconds slipping away haunted me until a colleague thrust her phone toward me - CalcMed: Urgência e Emergência glowed on the screen. Seven days free trial felt like a lifeline thrown to a drowning medic. Within minutes, I'd corrected the potassium deficit while simultaneously calculating vasopressor rates. This wasn't just another app - it transformed panic into precision when lives hung in the balance.
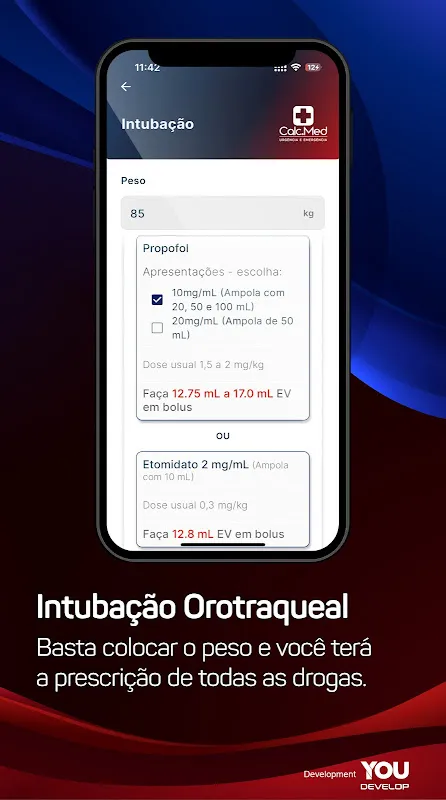
Orotracheal Intubation Protocols became my midnight guardian. When twin trauma victims arrived post-accident, their swollen airways demanded rapid sequence intubation. Instead of mental gymnastics recalling sedative doses, I tapped the section while prepping blades. The relief was visceral when etomidate and succinylcholine dosages appeared instantly, customized to their weights. No frantic page-turning, just cold steel in one hand and calculated certainty in the other.
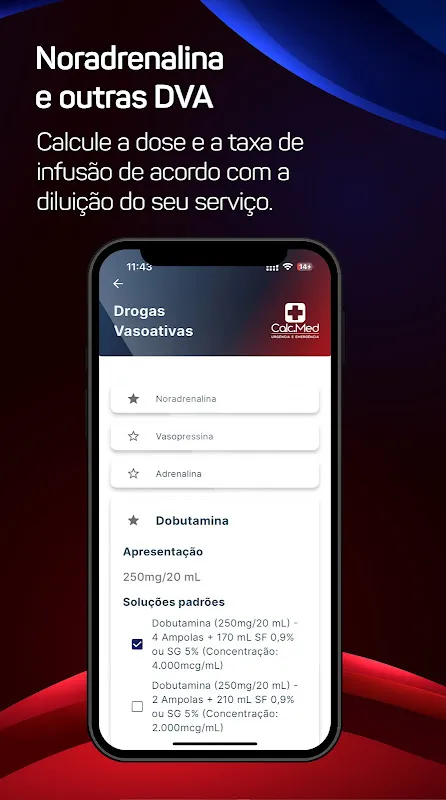
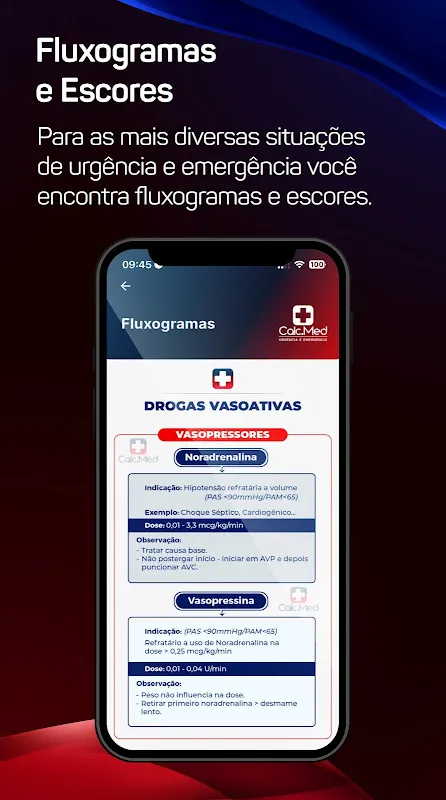
Vasoactive Drug Mastery rewired my night shifts. Picture this: 3 AM, septic shock patient with pressure nosediving. Sweat beaded on my forehead as I juggled norepinephrine lines. CalcMed's infusion speed calculator did what years of experience couldn't - eliminated dosage guesswork. The moment I adjusted the drip based on its micrograms/kg/min guidance, the monitor's shrill flatline warning softened to steady beeps. That mechanical symphony sounded like victory.
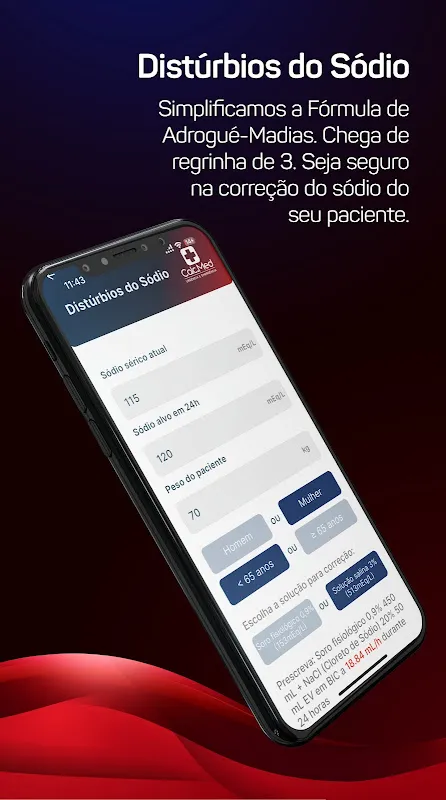
Electrolyte Correction Algorithms saved my rural rotation. Miles from lab support, a diabetic ketoacidosis case presented with sodium confusion. While nurses scrambled for IV bags, I input the values and watched it generate bicarbonate replacement math like a chemist over my shoulder. The satisfaction came hours later when blood gases normalized - not from luck, but because the app accounted for anion gap and fluid status in its wizardry.
Thrombolysis Dosing turned code greys into clear action. During a stroke alert last Tuesday, the weight-based alteplase calculator eliminated precious minutes of dosage debates. As the clock ticked past the golden hour, having thrombolysis meds broken down by kilogram with administration notes felt like an extra clinician scrubbing in. The patient's returning grip strength next morning was our shared triumph.
Wednesday 14:30, ICU round chaos. My attending fired creatinine levels like pop quizzes while the resident froze. With three taps, I had clearance calculations comparing Cockcroft-Gault to CKD-EPI - the gentle vibration confirming results felt like an academic high-five. Later, converting units for a pediatric transfer, the measurement converter handled lbs-to-kg and mcg-to-mg while ambulance sirens wailed. These tools don't just assist; they armor you against uncertainty.
Saturday 23:00, exhaustion setting in. Polarizing solution prep for an unstable cardiac patient usually means math-induced migraines. Instead, standardized solution guides walked me through amiodarone dilutions like a seasoned pharmacist murmuring ratios. That rare moment of mental stillness amid crisis? Priceless. The blog's latest post on vasopressor weaning later became my subway read, turning commute dead time into clinical growth.
The brilliance? Launch speed - faster than unboxing a syringe during a code blue. But perfection remains elusive: during a thunderstorm-induced power outage, I craved offline PDF exports for essential protocols. And while the annual plan saves coffeeshop money, I wish institutions covered subscriptions like stethoscopes. Still, when code carts fail and textbooks gather dust, this digital toolkit shines. For residents drowning in cross-cover nights or flight medics without backup, it's non-negotiable. Keep it charged beside your trauma shears.
Keywords: medical calculator, emergency medicine, critical care, drug dosing, clinical decision support