Chartnote Mobile: Voice-Powered Clinical Documentation Revolution
Staring at the clock after my 14th patient visit, panic set in knowing hours of charting awaited. That sinking feeling vanished when a colleague whispered about Chartnote Mobile. From the first dictation, I felt the weight lift - finally, an ally against paperwork mountains allowing genuine focus on healing hands.
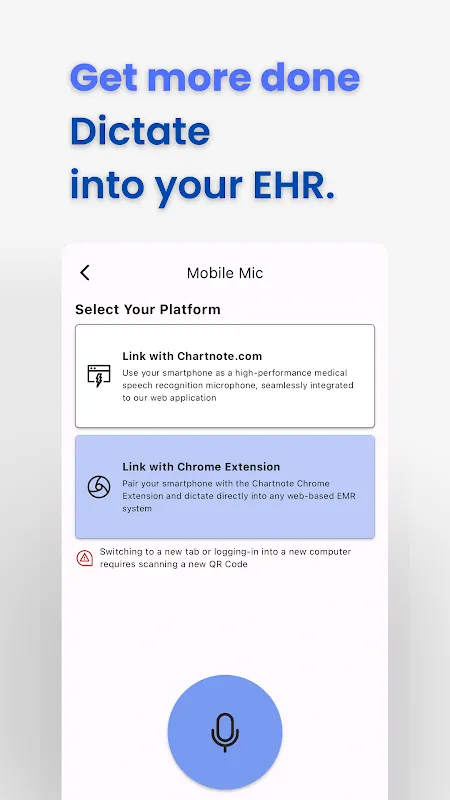
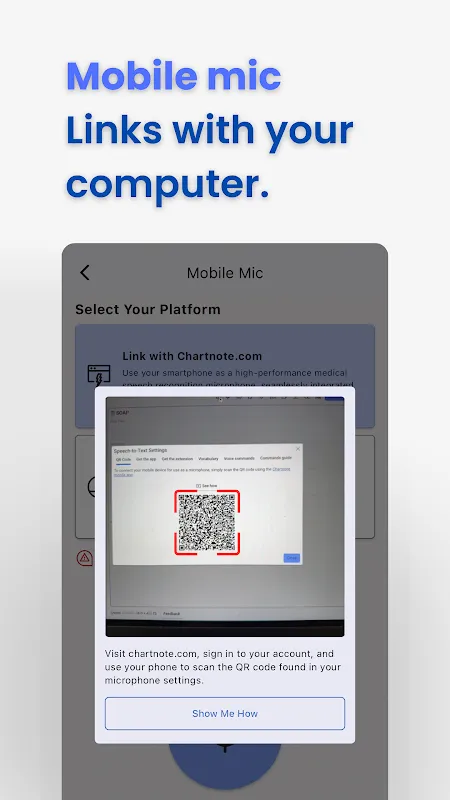
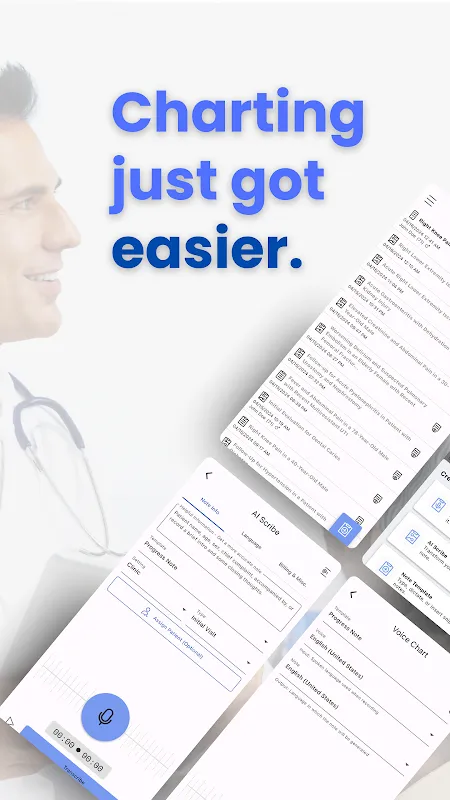
Voice ChartWhen Mr. Henderson described his complex symptoms, I tapped the mic icon mid-consultation. Watching his words transform into text in real-time felt like unlocking forbidden magic. That evening, replaying the recording revealed subtle cough nuances my tired ears had missed during the day's chaos.
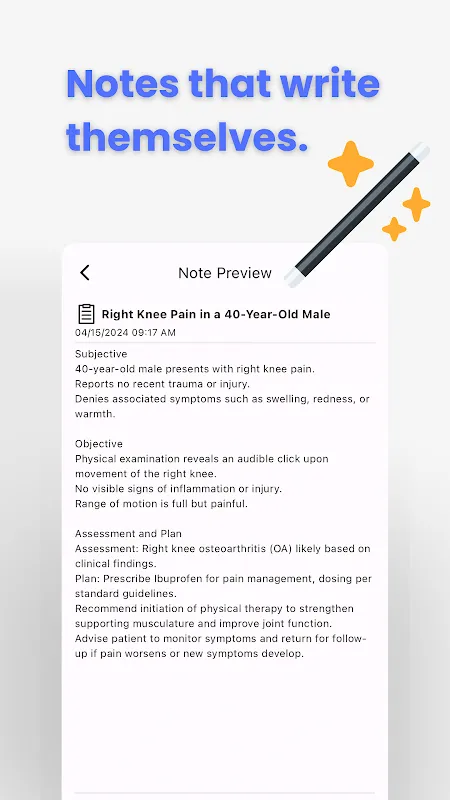
AI ScribeAfter urgent appendectomy notes piled up, I tentatively activated the AI. The generated draft perfectly structured operative findings with correct medical terminology. Now I routinely sip coffee while it organizes my scattered thoughts, like having a tireless resident working overnight.
Templates & SnippetsCreating custom templates for pediatric asthma cases became my secret weapon. Last Tuesday morning, inserting premade assessment blocks felt like deploying clinical cheat codes. When flu season hit, my customized snippet library saved 23 minutes per patient - time reclaimed for actual diagnostics.
Speech-to-TextDuring wound rounds, describing purulent drainage while gloved hands remained sterile seemed impossible until continuous dictation kicked in. The accuracy even captured "foul-smelling serosanguinous exudate" flawlessly. Now I verbally add lab correlations during walks between wards, feeling the satisfying click of efficiency.
Tuesday 7:08 AM: Sunrise glints off the ICU workstation as I murmur morning assessments. Chartnote's blue waveform pulses like a heartbeat, transcribing febrile symptoms between monitor alarms. That familiar relief washes over me - no more deciphering rushed handwriting before rounds.
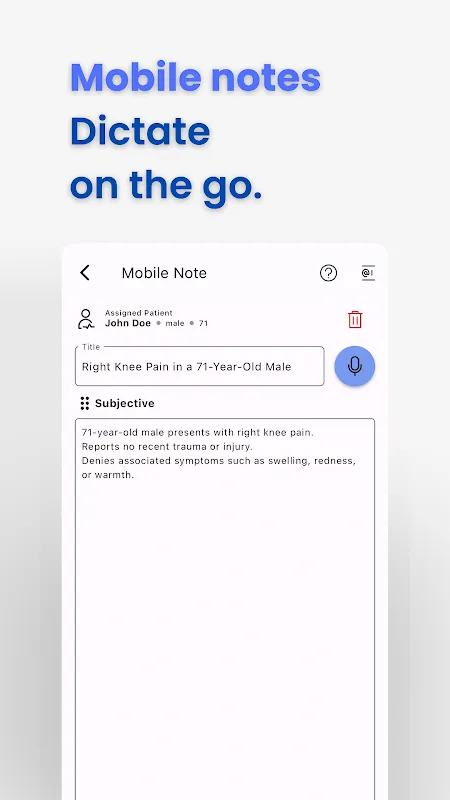
3:15 PM consult: Fractured hip patient moaning in pain. One-handed phone grip, verbalizing opioid orders directly into treatment plans. The immediacy prevents dosage errors I've seen with delayed charting. Later, the discharge summary auto-populates from snippets while I comfort the family.
11:20 PM home office: Reviewing AI-generated notes, I wince recalling that stubborn transcription glitch during ER chaos. Background noise occasionally scrambles medical abbreviations - fixable with manual edits but disruptive during codes. Still, launching faster than my hospital's EMR makes it indispensable. For clinicians drowning in documentation, this is the lifeline we've prayed for.
Keywords: clinical documentation, medical transcription, AI scribe, healthcare efficiency, voice recognition