Verpleegk Zorgresultaten NOC App: Evidence Based Nursing Outcomes at Your Fingertips
Staring at my patient’s complex chart after a 12-hour shift, I felt that familiar frustration—how do I objectively measure wound healing progress when fatigue clouds judgment? That’s when a colleague swiped open this Dutch-translated NOC app. Within minutes, I was crafting precise outcome indicators with terminology that finally bridged textbook theory and my exhausted reality. Designed for nurses drowning in documentation yet starved for clinical precision, this isn’t just another reference tool—it’s the compass I wish I’d had during my first year in oncology.
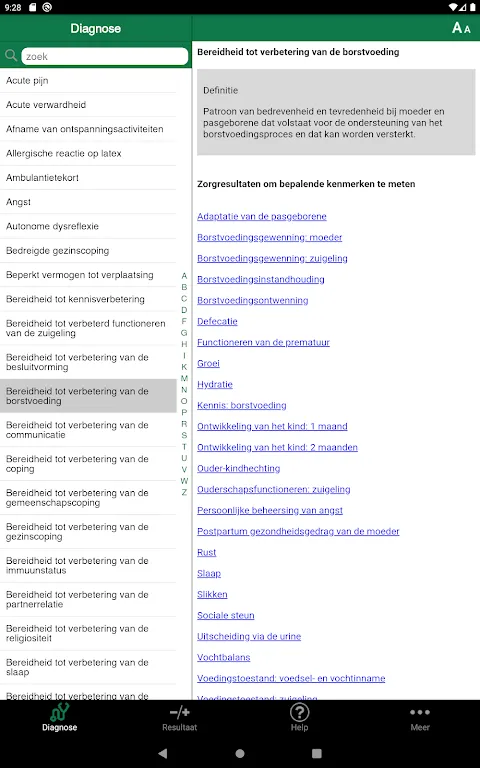
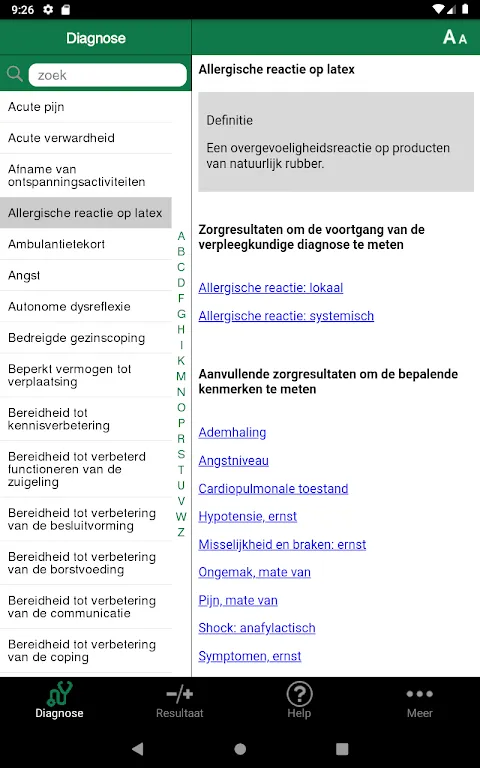
Comprehensive Outcome Library transformed my palliative care documentation. Last Tuesday, when Mrs. Janssen’s family asked about comfort metrics, I instantly pulled up the 540 updated outcomes. Scrolling through the 52 entirely new entries felt like discovering hidden pathways—especially the revised pain resilience scales. My finger paused at "End-of-Life Comfort" as validation washed over me: finally, terminology capturing what we witness but struggle to quantify.
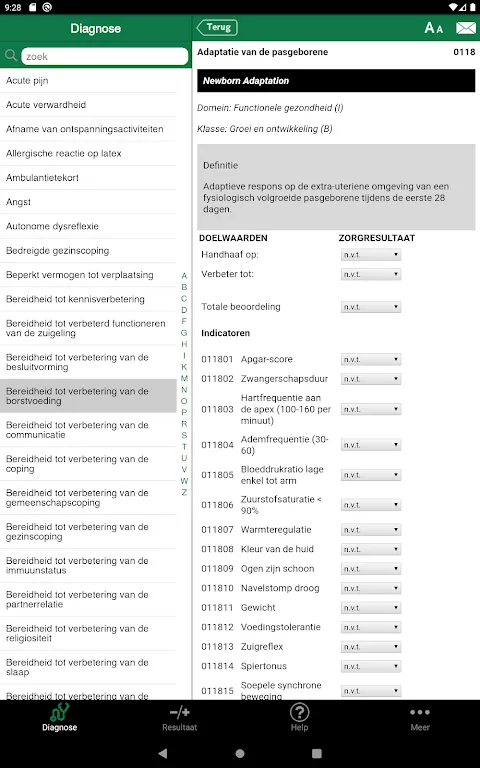
Evidence Based Structure became my shield during interdisciplinary rounds. When a resident questioned my mobility intervention plan, I tapped the research-linked rationale. Watching his skeptical expression shift to nod felt like warm sunlight breaking through hospital fluorescents—no more defensive explanations, just collaborative confidence rooted in data.
NANDA Diagnosis Integration saved me during a chaotic night shift. After triaging a COPD exacerbation, I linked "Ineffective Airway Clearance" to measurable respiratory outcomes in three swipes. That seamless pairing—like puzzle pieces clicking—meant I could act before the monitor alarms screamed, my pulse steadying as I adjusted oxygen protocols.
Discipline Adaptive Frameworks shine in home health visits. At Mr. De Vries’ farmhouse yesterday, I switched from geriatric to post-surgical modes while assessing his knee replacement. The interface intuitively adapted—no more awkward scrolling through irrelevant pediatrics metrics. That contextual intelligence? It’s the quiet colleague who anticipates your needs before you speak.
Rain lashed against the ambulance windows at 2 AM last Thursday. Paramedics rattled off stats while I balanced my tablet—one hand stabilizing the IV line, the other searching "Trauma Response" outcomes. The app’s clinical clarity cut through the adrenaline fog. Each tap resonated like a metronome keeping time amid chaos, turning gurney jolts into focused action steps.
What sings? Launch speed rivals emergency pagers—vital when sepsis protocols demand instant outcome mapping. The field-tested structure feels like worn leather gloves: flexible yet protective. But during pediatric codes, I crave customizable sound alerts—imagine harp tones escalating with critical indicators. Still, watching students use it to align curricula with clinical realities? That’s the quiet magic. Essential for nurses who measure progress in heartbeats, not spreadsheets.
Keywords: Nursing outcomes, evidence based, clinical decision, care planning, healthcare standardization