Midnight Musings with a Digital Nursing Sidekick
Midnight Musings with a Digital Nursing Sidekick
Rain lashed against the hospital windows as I slumped in the dimly lit charting room. My fingers trembled over Mrs. Henderson's wound documentation – a Stage IV pressure ulcer that mocked my exhausted attempts to quantify its angry crimson edges. Twelve hours into my oncology night shift, the coffee had stopped working hours ago, and the familiar dread crept in: how could I translate this weeping, complex reality into cold clinical data? That's when my phone vibrated – not a notification, but a deliberate lifeline. Earlier that evening, Clara from dayshift had pressed her personal device into my palm. "Try this when words fail you," she'd whispered conspiratorially. Now, with trembling thumbs, I tapped the unfamiliar blue icon.
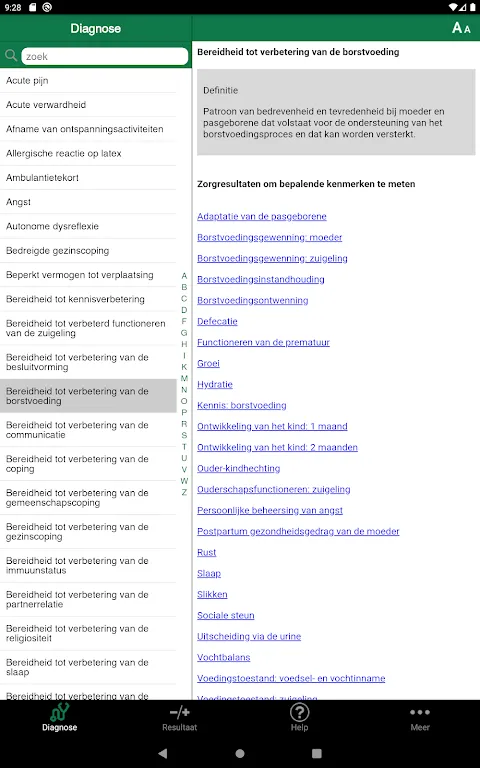
What unfolded felt like witchcraft. Instead of scrolling through endless dropdown menus, the interface presented me with visual progression scales that mirrored exactly what haunted my weary eyes. I could almost smell the sterile dressing as I matched wound characteristics to photographic benchmarks – granulation tissue percentage, exudate viscosity levels, even the precise shade of erythema. My pencil hovered over the paper chart as the app calculated a composite score in real-time, transforming subjective despair into quantifiable metrics. For the first time in months, I didn't feel like I was betraying the patient's suffering with inadequate documentation.
The true revelation came at 3 AM during change-of-shift handoff. When Dr. Reynolds challenged my assessment of "slight improvement," I didn't flounder. With two taps, I projected the app's comparison overlay – last week's wound perimeter superimposed over today's image, annotated with millimeter-precise shrinkage indicators. His skeptical eyebrows lifted as the algorithmic trend analysis projected healing trajectories based on tissue oxygenation data we'd inputted hourly. "Well," he muttered, adjusting his glasses, "can't argue with math." That moment tasted like victory – bitter and sweet – dissolving the usual physician-nurse power dynamic in a single swipe.
Yet this digital savior wasn't flawless. During Mrs. Henderson's dressing change, my latex-gloved fingers fumbled with the tablet's touchscreen. The app demanded photographic evidence under specific lighting conditions – impossible when wrestling with adhesive borders and a restless patient. I cursed as it rejected three consecutive images for "suboptimal contrast," forcing me to repeat the painful procedure. Later, its insistence on documenting psychosocial impact metrics felt grotesque when all Mrs. Henderson could whisper was "please make it stop." The algorithm couldn't quantify dignity, only simulate empathy through pre-programmed dropdowns about "patient verbalized distress."
Dawn found me weeping in the supply closet – not from exhaustion, but because the app's shift summary revealed what my denial had obscured: despite heroic interventions, the necrosis progression curve was accelerating. The brutal mathematics spared no feelings, its predictive analytics more honest than any comforting lie I might have told myself. When I finally showed the trajectory graph to Mrs. Henderson's daughter, the raw data accomplished what my rehearsed speeches never could – permission to pivot toward palliative care. We cried together over bar charts and heat maps, the clinical detachment somehow making space for human grief.
Keywords:NOC Outcomes App,news,oncology nursing,wound documentation,clinical algorithms









