2 AM Panic and the App That Answered
2 AM Panic and the App That Answered
Rain lashed against the window like thrown gravel as I pressed my palm against my daughter’s forehead. Burning. The thermometer confirmed it: 103°F. That primal dread coiled in my stomach—the kind only parents know when their child’s breath comes in shallow rasps at midnight. Our local clinic’s phone line played a cruel symphony of hold music for 20 minutes before disconnecting. I’d have driven to the emergency room if not for the slick roads and her worsening chills. Then I remembered a colleague’s offhand remark about digital triage tools during a coffee break. Desperation makes you try anything.
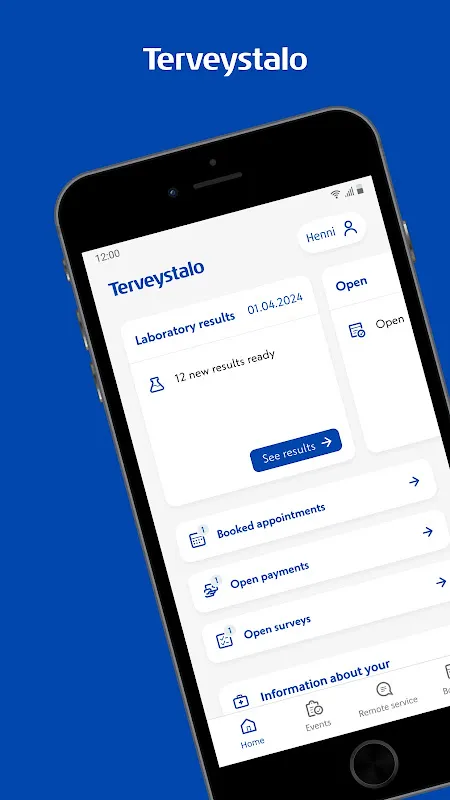
Downloading felt like fumbling in the dark. My hands shook typing my name. But within minutes, I was staring at a calm interface asking symptom details: fever duration, breathing patterns, rashes. It didn’t just collect data—it analyzed. A progress bar filled as it cross-referenced pediatric guidelines, and then, a soft chime: "Urgent video consult available with Dr. Aava." Relief washed over me so violently I nearly dropped the phone. Behind that feature lay algorithmic urgency-scoring—prioritizing cases by vital risk factors invisible to users. No human operator could’ve matched that speed.
The video call connected instantly. Dr. Aava’s face appeared, framed by a bookshelf, her voice steady despite the hour. "Show me her throat, please." As my daughter whimpered, the app’s real-time diagnostic support subtly aided the doctor—highlighting possible strep indicators based on our input. I later learned it used machine learning trained on thousands of pediatric cases. But in that moment? It felt like a lifeline. The prescription for antibiotics flashed on-screen instantly, along with a map showing the only 24-hour pharmacy 12 miles away. Yet here’s where the magic cracked: the e-prescription failed to auto-send. I had to manually show the barcode at the counter, wasting precious minutes while my partner stayed with our shivering girl. For an app boasting seamless integration, that glitch stung like betrayal.
Driving through stormy darkness, I craved the app’s cold efficiency again. Post-consultation, it transformed into a nurse-like companion: dosage timers, fever-logging charts, even hydration reminders syncing across our devices. But its true genius was in the unspoken—how its predictive symptom tracker flagged "unusual fatigue patterns" days later, prompting an early follow-up that caught secondary ear inflammation. Most platforms just store records; this one anticipated crises. Still, I cursed its medication database when it couldn’t identify our local pharmacy’s generic antibiotic brand, leaving me deciphering chemical names under fluorescent lights at 3 AM. Perfect? Hell no. Indispensable? Absolutely.
Weeks later, I caught myself using it for my own migraines. The way it remembers your history—not just as data points, but as a narrative—feels eerily human. Input "throbbing temple pain + light sensitivity," and it recalls your past triggers, suggests hydration based on weather data, and even dims your screen automatically. That’s not coding; it’s digital empathy. Yet I rage-quit once when its "instant booking" feature offered slots 3 days out during peak flu season. For all its AI brilliance, demand overwhelmed its supply logic. You can’t algorithm away doctor shortages.
Now it lives on my home screen—a quiet guardian. I no longer panic at midnight fevers. But I’ve learned its rhythms: trust its diagnostics, double-check its pharmacy links, and never assume seamless means flawless. That stormy night taught me modern healthcare isn’t about replacing humans; it’s about apps like this bridging the terrifying gaps when humans can’t reach you. My daughter’s recovered. My anxiety hasn’t. But when she coughs at 2 AM? My fingers already hover over the icon. Imperfect, impatient, indispensable.
Keywords:Terveystalo,news,telemedicine,parenting emergencies,digital triage









