Code Blue Guardian: My Drug Guide Lifeline
Code Blue Guardian: My Drug Guide Lifeline
My stethoscope felt like an iron weight against my chest during that midnight rapid response call. Mrs. Henderson's O2 stats plummeted as her IV pump beeped relentlessly - another failed beta-blocker infusion. "Possible amiodarone interaction?" the resident barked while prepping the crash cart. My mind went terrifyingly blank, that familiar acid burn creeping up my throat. Then Jenna's cracked phone screen flashed alive beside me. Three taps. A scroll. "Contraindicated with class III antiarrhythmics - risk of prolonged QT interval!" she snapped. That glowing rectangle became our anchor in the storm, its clinical precision cutting through the chaos like surgical steel.
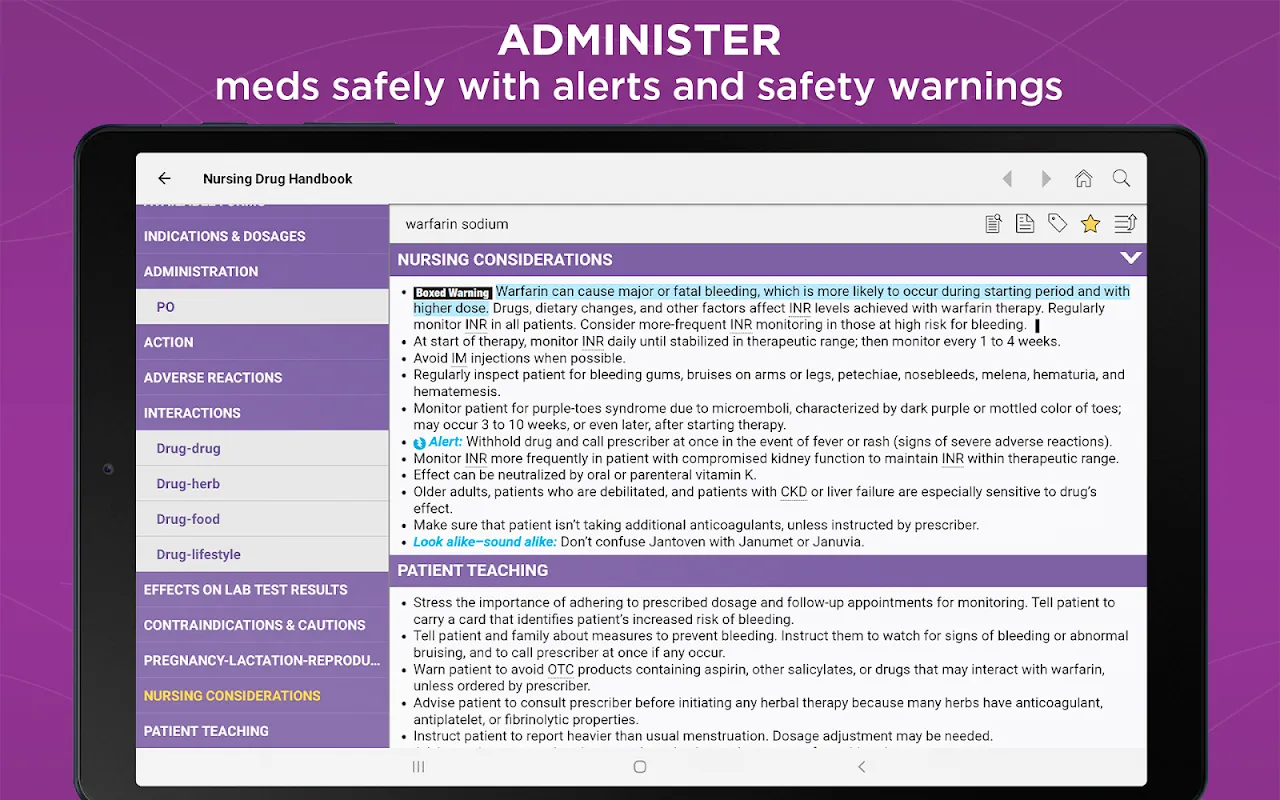
What Jenna wielded wasn't just another medical app - it was a living pharmacopeia reborn as Nursing Drug Handbook 2024. When I downloaded it that night, trembling fingers smudging my screen, I discovered why seasoned nurses called it "the pocket attending." The search function anticipated my typos before I finished misspelling "levetiracetam." Offline access meant no more praying for signal in elevator dead zones. But the true witchcraft? How it transformed dense monographs into action bullet points during med passes. Suddenly I wasn't just administering furosemide - I knew exactly which electrolyte imbalances to watch for when Mr. Davies started trembling.
This digital oracle spoiled me rotten. Remembering the dog-eared paper reference we used to fight over at the nurses' station feels like recalling dial-up internet. That clumsy tome couldn't auto-update when the FDA slapped black box warnings on our most prescribed antibiotics last spring. Yet here's where my reverence meets reality: the app's interaction checker sometimes overzealously flags benign combos. I nearly caused a panic attack canceling Mr. Petrov's harmless calcium supplement before realizing the algorithm misfired. And don't get me started on the subscription cost - paying nearly half my CNA's hourly wage for annual access stings when hospital budgets bleed us dry.
Late Tuesday shifts became my testing ground. Between 2am delirium and cafeteria coffee, I'd pit the app against our EMR's built-in database. Watching it demolish our clunky hospital software in speed trials felt illicitly satisfying - like bringing a scalpel to a butter knife fight. The secret sauce? Its developers harnessed cloud-synced clinical repositories that update while we sleep. When new sepsis protocols dropped last quarter, my phone buzzed with push notifications before administration's memo hit our inboxes. This constant evolution makes it feel less like software and more like a symbiotic clinical partner.
Criticism claws its way back during crash course orientations. Watching baby nurses blindly trust dosage calculators without cross-referencing PI sheets makes my knuckles whiten. Last month, a new grad nearly titrated warfarin based solely on the app's renal adjustment tool - forgetting the patient's recent liver biopsy. Technology shouldn't replace critical thinking; it should fuel it. Yet when I caught the error, guess what we used to explain the hepatic metabolism pathways? The irony wasn't lost on either of us.
Rain lashed against the ambulance bay windows during my most brutal test. Multiple trauma incoming - GSW, polypharmacy, unknown history. In the controlled chaos of triage, I scanned med lists while simultaneously calculating drip rates. The app's split-screen feature became my lifeline, monographs for morphine and ketamine glowing side-by-side as I prepped concurrent lines. When the ER doc questioned my dilution ratios, I flipped the screen toward him: "See? 1mg/mL in NS compatible per updated compatibility charts." His nod was all the validation I needed. In that moment, the app ceased being mere software and became an extension of my nursing intuition.
Does it make me complacent? Sometimes. When the dopamine drip alarms screamed last Thursday, I reached for my phone before checking the IV site - a dangerous reflex. But as my fingers hovered over the troubleshooting guide, muscle memory kicked in. The extra second I gained from not fumbling through paper indexes let me spot the infiltrated line immediately. That's the paradox: this tool simultaneously challenges and enhances my instincts. Now it sleeps nestled between my badge and hemostats - a digital talisman against uncertainty. When fresh grads ask about essential gear, I still say "good shoes and better instincts." But my eyes always flick to that chipped phone case. Some lifelines fit in your pocket.
Keywords:Nursing Drug Handbook 2024,news,medication safety,clinical decision support,emergency pharmacology









