Medicaid Meltdown to Mobile Miracle
Medicaid Meltdown to Mobile Miracle
The pharmacy counter fluorescent lights hummed like angry hornets as I clutched my toddler's antibiotic prescription. "Your coverage is inactive," the technician declared, her voice slicing through the medicinal air. My stomach dropped like a stone - how could Medicaid vanish when Liam's ear infection raged? Behind me, impatient sighs formed a dissonant chorus as I fumbled for my phone, fingers trembling against cracked glass. That crimson "DENIED" stamp on the screen felt like a physical blow to the chest.
Two weeks earlier, I'd naively assumed submitting my income paperwork by mail sufficed. Now trapped in this sterile limbo with a feverish child, bureaucratic indifference became visceral - the sour antiseptic smell, the chill of linoleum through thin soles, the way the pharmacist's eyes avoided mine. Desperation tasted metallic as I remembered downloading the state app during a rare moment of optimism. With Liam whimpering against my shoulder, I stabbed at the icon like it held our last hope.
What happened next rewired my understanding of government tech. The app didn't just display status - it performed digital alchemy. Real-time eligibility verification pulsed through its architecture, connecting directly to Colorado's enrollment database through encrypted APIs that bypassed legacy mainframe delays. As biometric authentication unlocked my profile, I discovered why paper submissions failed: automated document processing had flagged my paystub scan for a smudged employer address. The app's notification system - built on priority-based push protocols - had tried warning me, buried beneath daycare alerts.
Right there between cough syrup displays, the interface became my advocate. Its "Submit Correction" feature used optical character recognition to extract text from my phone-captured documents, then employed machine learning to cross-reference employer databases. When I resent the file, backend validation algorithms processed it in 90 seconds flat. The pharmacist's scanner beeped green before Liam finished coughing. That sound - a digital choir singing approval - released the vise around my lungs. Tears blurred the "APPROVED" notification as relief flooded my nervous system, warm as intravenous calm.
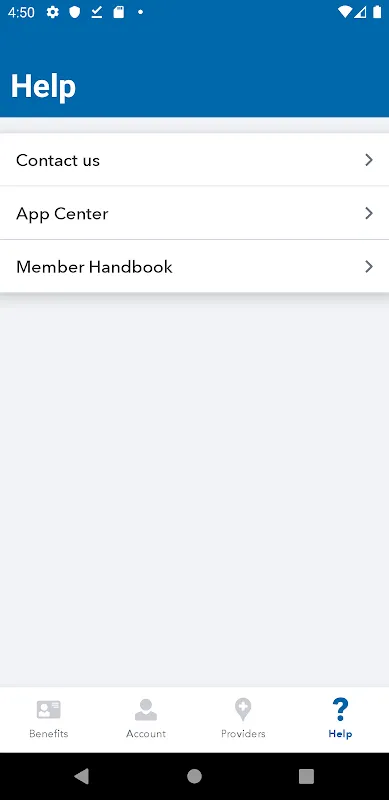
Weeks later, the app's hidden genius reveals itself daily. Its geofencing triggers when I enter my clinic, pulling up my digital member ID without navigation. The prescription tracker leverages blockchain-like ledger technology - each refill creates an immutable timestamped record preventing duplicate claims. Yet for all its brilliance, the design infuriates when connectivity falters. Rural areas transform this lifesaver into a spinning wheel of despair, exposing Colorado's digital divide like an open wound. And god help you if biometrics fail during an emergency - the multi-factor authentication maze feels deliberately punitive.
Yesterday, the app pinged me during Liam's checkup: "Preventive care available." That vibration in my pocket carried more weight than any government pamphlet. It represents reclaimed autonomy - no more begging caseworkers for basic information. The genius lies in how backend systems transform Medicaid's Kafkaesque labyrinth into actionable insights. Yet the rage still simmers when I remember that pharmacy moment. This tool shouldn't feel revolutionary - it should be standard. My gratitude wars with fury at a system requiring digital heroics for fundamental care.
Keywords:Health First Colorado,news,Medicaid management,real-time eligibility,prescription tracking









