My Cabin Crisis Turned Virtual Lifeline
My Cabin Crisis Turned Virtual Lifeline
Rain lashed against the windowpane of my remote mountain cabin last Sunday, the fireplace crackling as I finally relaxed with my first coffee in weeks. That peace shattered when my phone screamed with a code blue alert from the hospital. Mrs. Henderson - my 72-year-old diabetic patient recovering from bypass surgery - was crashing. Miles from my clinic, that familiar icy dread clawed at my throat as I imagined her chart buried under discharge papers back at the office.
Fumbling with my laptop, I nearly knocked over my mug. Then I remembered the emergency protocols we'd set up in that telemedicine platform our group started using. My trembling fingers punched in the credentials, and within seconds, Mrs. Henderson's entire medical history materialized onscreen. There it was: her abnormal electrolyte panel from yesterday that I'd flagged remotely. The app's real-time vitals integration showed her potassium levels spiking off the charts. How had the night staff missed this?
I initiated a video consult right through the dashboard, my breath fogging the camera lens as I barked orders to the flustered resident. "Stop the IV fluids immediately! Administer calcium gluconate and prep insulin!" Watching the live EKG stabilize on my split-screen felt like defusing a bomb with surgical gloves on. The resident's panicked eyes met mine through the pixelated feed as the waveform steadied. That moment when her O2 saturation climbed back to 95%? I tasted copper in my mouth from biting my cheek too hard.
What saved us wasn't just the video functionality - it was how the damn thing anticipates chaos. While managing the crisis, the platform automatically logged every action with timestamps and generated incident reports. Its automated audit trails captured medication orders and nurse acknowledgments without me lifting a finger. Later, reviewing the encrypted session logs felt like rewatching a horror movie where I already knew the hero survived.
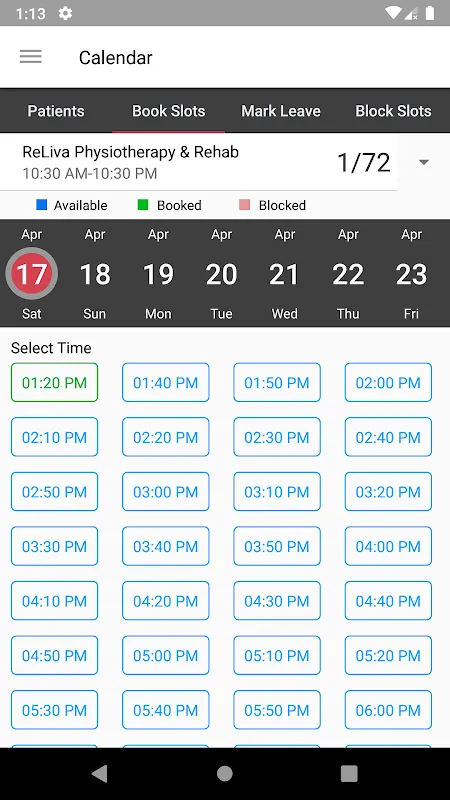
Post-crisis, the real magic happened. The scheduling module detected the disrupted follow-up plan and rebuilt Mrs. Henderson's entire care pathway around this emergency. It rescheduled her cardiac rehab, adjusted medication reminders, and even pinged dietary services - all while I was still shaking in my damp hiking socks. This wasn't some robotic auto-scheduler; it understood that her new insulin sensitivity required endocrinology consults the original plan didn't include.
Now here's where I curse this beautiful monstrosity. That same algorithmic efficiency becomes tyrannical when you're exhausted. At 2 AM last night, its notification chime jolted me awake - "URGENT: Patient John Rivera missed hypertension meds." My sleep-deprived rage peaked discovering it was just a system-generated alert about refill delays. No human would've escalated that nonsense. The app's overzealous machine learning sometimes forgets clinicians need oxygen too.
Still, stumbling back to bed, I grudgingly admired how its architecture handles vulnerability. Unlike those consumer telehealth apps leaking data like sieves, this fortress uses zero-knowledge encryption that even IT can't bypass. When I access records, it feels like entering a biometric vault - retinal scans would be less secure. My paranoid cardiologist self finally sleeps knowing no hacker can intercept my prescriptions between server hops.
Watching dawn break over the mountains now, coffee in hand again, I realize this platform hasn't just changed how I practice - it's rewired my instincts. That visceral panic when alerts sound has been replaced by a cool, almost predatory focus. My stethoscope gathers dust on the cabin desk while my laptop hums with six active patient dashboards. The irony? Technology meant to create distance has me feeling more connected to Mrs. Henderson's beating heart than ever before.
Keywords:MH DoctorVC,news,telemedicine crisis,clinical workflow automation,patient data security









