My Cardiac Lifeline in a Pocket
My Cardiac Lifeline in a Pocket
The alarm shattered my pre-dawn stillness – Code Blue, Cath Lab Stat. I stumbled into scrubs, adrenaline sour on my tongue, knowing Mr. Henderson awaited with his failing heart and that damned mystery pacemaker. His old records were lost in some paper purgatory, and the clock ticked like a detonator. Sweat glued my gloves as I fumbled through outdated manufacturer binders, each page a Rorschach test of indecipherable serial numbers. My fingers trembled over the crash cart when I remembered the icon buried in my phone: iPacemaker Device. One frantic scan of his device ID later, the screen blazed to life – not just model specs, but a full interrogation report showing his lead integrity was hanging by a thread. That crimson warning probably saved us both a trip to the morgue.
When Milliseconds Morph Into Lifetimes
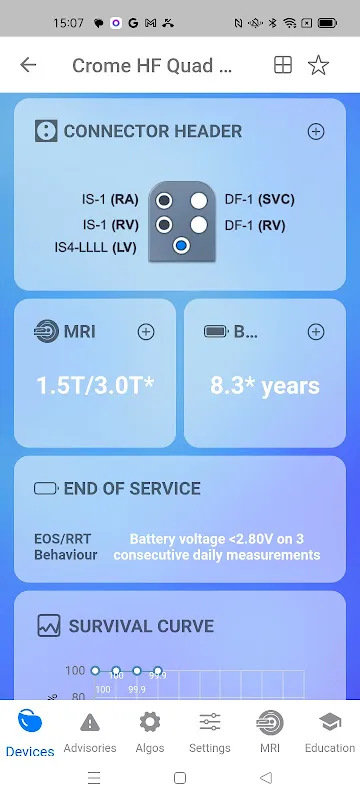
What feels like witchcraft is actually brutal database engineering. The app doesn't just regurgitate PDF manuals – it cross-references proprietary encryption from six major manufacturers against real-time clinical data streams. That MRI compatibility checker? It doesn't just spit out "yes/no." Last Thursday, it mapped Gina Lopez's implant against her specific scanner's magnetic field gradient, flagging that her abandoned lead fragment would overheat at 1.5 Tesla. The algorithm visualized thermal dispersion patterns in a 3D overlay that made our physicist whistle. Yet for all its brilliance, the interface fights you like a rabid raccoon when updating patient histories. Why must I triple-tap to log generator replacements? That UX designer deserves cardiac monitoring – of the punitive kind.
Ghosts in the Machine
I've developed rituals with this digital partner. Before high-risk procedures, I whisper serial numbers into my phone like incantations. The app rewards me with surgical histories deeper than FBI dossiers – recall notices, impedance trends, even battery depletion curves predicting failure within 48-hour windows. But when cell service flickers in our basement lab? The app transforms into a petulant toddler, freezing mid-interrogation. That outage during the Thompson case cost us eleven minutes of ventricular tachycardia while I sprinted upstairs for Wi-Fi. No offline cache? In 2023? That's not oversight – it's medical negligence coded in Python.
The true horror emerged with pediatric implants. Tiny devices with nano-engineered components behave unpredictably – which this platform acknowledges with terrifying honesty. When inputting little Chloe's Micra AV, the app didn't pretend omniscience. Its uncertainty algorithm painted confidence intervals in pulsing amber zones around MRI safety parameters. We postponed her scan, dug deeper, and discovered her off-label implant configuration could've triggered lead displacement. That humility – that admission of limitations – is rarer than platinum electrodes. Still, I curse its notification system daily. Priority alerts for critical recalls get buried beneath promotional spam about subscription tiers. Somewhere, a marketing ghoul is high-fiving Satan.
Code Blue for Common Sense
Last full moon, it happened. Code STEMI at 3AM, patient screaming in Spanish, old pacemaker buzzing like a broken fridge. My resident froze, eyes darting between the erratic rhythm strip and a German manual. I slammed the phone against the crash cart – scan complete – and the app exploded with warnings: electromagnetic interference threshold exceeded by our new ablation generator. We killed the machine mid-shock, switched to bipolar forceps, and avoided frying his device into a charcoal briquette. Later, reviewing the case, we discovered the app had logged the near-disaster in its incident registry – anonymously feeding data back to manufacturers. That silent, perpetual loop of improvement haunts me. How many deaths did it prevent today while I drank bad coffee?
Yet I rage against its corporate shackles. Why can't I integrate it with our EP lab's mapping systems without jumping through HIPAA hoops that require blood sacrifices to compliance officers? The raw power exists – I've seen the API documentation – but accessing it feels like negotiating with drug cartels. Every feature request vanishes into ticket-system oblivion unless accompanied by institutional purchase orders. For frontline clinicians? We get sticker-shock from premium tiers while wrestling with free-version limitations that feel deliberately sadistic.
Static Electricity and Second Chances
This morning, I found myself stroking my phone like a talisman before implanting a new Biotronik system. Not for the specs – I know those cold – but for the app's complication predictor. It analyzed the patient's osteoporosis scans and warned of higher perforation risk with standard screw-in leads. We switched to a suture-fixation model, avoiding what could've been a catastrophic right ventricle puncture. Later, scrubbing out, I realized I'd developed a new tic: unconsciously thumbing my pocket during consults, feeling for that rectangular lifeline. It's not perfect – god, it's infuriatingly flawed – but when the ECG flatlines and history vanishes, this glitchy rectangle holds more clinical truth than entire hospital archives. Just please, for love of all that's holy, fix the damn offline mode.
Keywords:iPacemaker Device,news,cardiac implant safety,MRI compatibility,clinical decision support









