My Digital Lifeline in the Midnight Hour
My Digital Lifeline in the Midnight Hour
That Tuesday started with the kind of fatigue that turns bones to lead. By sunset, my throat felt lined with shattered glass while fever chills rattled my teeth like dice in a cup. Alone in my dim apartment, I stared at the thermometer's cruel 103.5°F glow - the exact moment panic began coiling around my ribs. Flu? COVID? Something worse? In that vulnerable darkness where rational thought dissolves, my trembling fingers found salvation: Phillips HMO Mobile.
What unfolded next still leaves me breathless. The app's emergency triage feature didn't just ask symptoms - it listened. Using adaptive questioning algorithms that narrowed possibilities with each response, it transformed my garbled fears into clinical clarity. When I described the stabbing pain behind my sternum, its machine learning engine cross-referenced my medical history and flagged potential pleurisy. This wasn't some WebMD horror generator - it weighted probabilities using real-time local infection data and my pre-existing conditions.
The Architecture of CalmWhat makes this technological marvel hum? Beneath its serene interface lies a federated data architecture pulling from disparate systems - hospital EHRs, pharmacy databases, even wearable metrics. When I authorized emergency access, it built a consolidated health snapshot in seconds: my last EKG readings, allergy alerts, even current medication interactions. That's when I noticed the subtle genius - while recommending urgent care, it simultaneously notified my primary physician through HL7-compliant messaging and reserved me a slot at an in-network clinic 12 minutes away. All without a single phone call.
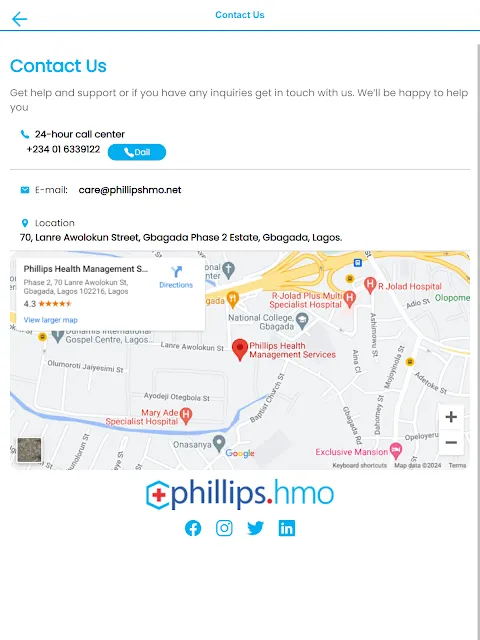
But technology reveals its true worth in friction points. My frantic Uber ride became a nightmare when the clinic's address failed to sync to my maps. Cursing the app through tear-blurred eyes, I discovered why - offline mode defaults were buried three menus deep. Yet redemption came swiftly: tapping "Share Records" generated a scannable QR code containing my entire medical profile. The intake nurse's eyes widened as she scanned it. "This usually takes 45 minutes of paperwork," she murmured, already wheeling me toward examination.
Beyond the Crisis HorizonRecovery became a masterclass in digital healthcare choreography. The app's medication tracker transformed my chaotic pill schedule into gentle nudges - complete with visual identifiers since my fogged brain couldn't remember "the small white one." But the real revelation was its biometric integration. Pairing with my fitness watch, it detected abnormal nocturnal heart rhythms and prompted me to capture ECGs during episodes. When irregularities persisted, its predictive analytics flagged potential post-viral pericarditis before my follow-up - arming my cardiologist with weeks of actionable data.
Let's not canonize it though. The "Wellness Challenges" module remains patronizing garbage - earning digital badges for hydration goals while recovering from cardiac inflammation felt like satire. And the telemedicine feature? During one video consult, compression artifacts made my swollen tonsils resemble abstract art. But these are quibbles against a tool that fundamentally altered my relationship with healthcare. Where once stood faceless bureaucracy now lives a responsive, almost intimate companion.
Weeks later, watching sunset paint my living room gold, I realize Phillips HMO Mobile rewrote my survival story. It didn't just connect dots between symptoms and solutions - it became the connective tissue. The quiet confidence when opening it now stems not from features, but from knowing its neural network of APIs and algorithms stands guard in life's vulnerable moments. My insurance card gathers dust; this is where true coverage lives.
Keywords:Phillips HMO Mobile,news,healthcare technology,medical AI,chronic illness management









