My Digital Stethoscope: ethizo's Life-Saving Symphony
My Digital Stethoscope: ethizo's Life-Saving Symphony
The cardiac monitor's shrill alarm sliced through ICU's fluorescent hum as I fumbled between devices - tablet displaying incompatible lab results, phone vibrating with pharmacy queries, pager blinking with nursing station alerts. Sweat pooled beneath my collar as I mentally juggled Mr. Henderson's crashing vitals against three different login screens. This chaotic ballet of fragmented technology nearly cost lives daily until ethizo's ecosystem transformed my trembling fingers into a conductor's baton.
Remembering that first download feels like recalling CPR on my own career. The installation wizard asked permissions I'd normally deny - camera, microphone, location - until realizing it wasn't harvesting data but weaving a safety net. Granting access felt like handing over scalpel-sharp tools to a surgical robot: terrifying trust required. When the dashboard materialized, its minimalist design deceived me. Just five tabs - Patients, Communications, Resources, Scheduling, Billing - yet each unfolded like a nesting doll of clinical possibilities.
Last Tuesday's graveyard shift tested this digital transformation. Paramedics radioed ahead about an unresponsive teen OD'ing on synthetic opioids. Normally I'd waste precious minutes: shouting med requests across ER, manually calculating naloxone doses, hunting for toxicology protocols. Instead, The Synchronized Resuscitation unfolded through my smudged tablet screen. Facial recognition ID'd Jane Doe through ambulance photos while I scanned her QR-coded wristband. Instantly her ER bay lit up with projected allergies, baseline vitals, and real-time paramedic feeds. The app's drug interaction matrix flagged potential serotonin syndrome as I ordered diagnostics with voice commands - "Full tox screen, stat ABG, prep intubation" - each directive auto-logged and timestamped.
What truly stole my breath wasn't the technology but its invisible orchestra. While manually bagging Jane, my peripheral vision caught critical alerts: plummeting SpO2, rising lactate levels. The platform's predictive analytics had already suggested sepsis protocol and cross-matched blood products. I approved orders with knuckle-taps on the tablet edge - no sterile gloves removed. When her heart rhythm deteriorated, the app surfaced emergency cardiology contacts while simultaneously generating consent forms for her panicked parents via encrypted video. That seamless handoff between crisis management and human connection felt like discovering a new vital sign.
Yet this digital utopia reveals brutal edges. During last month's system update, prescription auto-fill malfunctioned mid-clinic. Twelve patients waited while I manually re-entered dosages, the app's cheerful notification - "Optimizing your experience!" - mocking my rising panic. And heaven help you when rural hospitals' ancient Wi-Fi falters; the offline mode resurrects 2010-era medicine with soul-crushing slowness. These fractures in the digital facade trigger primal dread - the terror of technological abandonment when lives hang in balance.
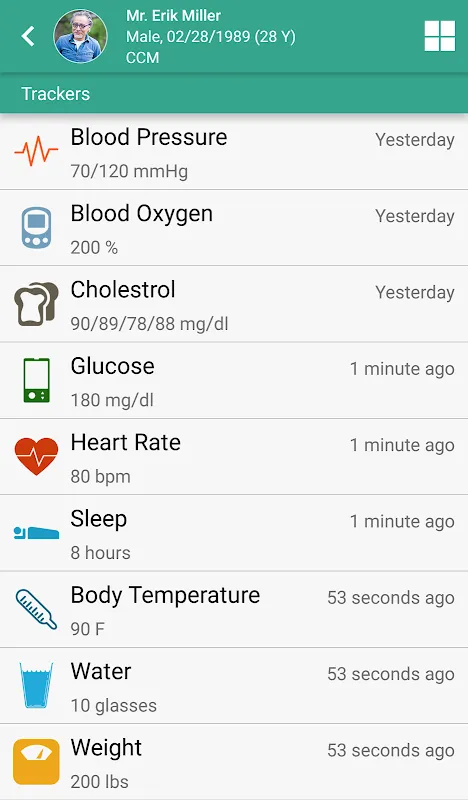
What haunts me most are the ghosts of pre-ethizo medicine. Yesterday I discovered Maria Rodriguez's diabetes management plan - not in some forgotten chart, but threaded through our year-long message history. The app had quietly mapped her HbA1c improvements against medication adjustments, lifestyle notes, even emoji-filled encouragements from her daughter. This longitudinal tapestry revealed patterns my exhausted brain had missed: glucose spikes consistently preceding full moons when her nightshift workload peaked. We adjusted her insulin regimen accordingly today - preventative care woven from digital breadcrumbs.
Critics dismiss such platforms as bureaucratic bloat, but they've never coded a patient in one hand while ordering life-saving meds with the other. The true magic lies in clinical choreography - how the app collapses time between diagnosis and intervention. Yesterday's ICU transfer proved this: as I narrated findings into the mic, the platform generated transfer summaries, auto-populated ambulance checklists, even alerted receiving physicians before I finished speaking. That precious eight-minute head start likely saved Mr. Petrov's ischemic bowel.
Still, I rage against its algorithmic arrogance. When end-of-life discussions appear as templated "care plan options," when grief-stricken families receive automated bereavement resources before I've pronounced time of death - these jarring moments reveal medicine's irreducible humanity. No app can replace the weight of my hand on a trembling shoulder, the deliberate silence after delivering catastrophic news. This tension between technological efficiency and tactile compassion forms medicine's new frontier.
Tonight as I review tomorrow's surgeries, the platform's ambient mode glows softly - a constellation of patient vitals across wards. Mrs. Chen's postoperative BP fluctuates; the app suggests PRN hydralazine while cross-referencing her renal function. I approve remotely, watching her numbers stabilize in real-time from my kitchen. This omnipresent vigilance should terrify me, yet it feels like finally having augmented clinical intuition. The machine doesn't replace judgment - it elevates it, turning scattered data points into symphonic diagnostics. When my pager inevitably shrieks again tonight, my hands won't shake searching for tools. They'll dance across a single screen conducting life-saving harmonies.
Keywords:ethizo Provider,news,medical technology,patient care,clinical efficiency








