My Midnight Panic Button: UnitedHealthcare's Lifeline
My Midnight Panic Button: UnitedHealthcare's Lifeline
Cold sweat trickled down my spine at 2:37 AM when that vise-like grip clamped around my chest. Alone in my apartment, fingers trembling too violently to dial 911 properly, I fumbled for my phone - not to call emergency services, but to open the digital lifesaver I'd ignored for months. The UnitedHealthcare app's glow cut through the darkness like a beacon as I gasped through what felt like an elephant sitting on my ribcage. That pulsating blue icon became my anchor in a tsunami of terror.
What happened next still leaves me breathless (though thankfully metaphorically now). With stabbing pains radiating down my left arm, I stabbed at the "Find Care" button. The app didn't just show nearby ERs - it calculated estimated wait times, co-pay costs, and even displayed which facilities had cardiac specialists on duty that exact moment. When it highlighted St. Vincent's just 1.2 miles away with a 7-minute average wait, I nearly wept with relief. That real-time data integration isn't just convenient - it's algorithmic triage that could mean the difference between cardiac muscle salvaged or lost.
The Code Beneath the Calm
What makes this different from googling "ER near me"? The app's backend hooks directly into United's claims processing system using HL7 FHIR APIs - healthcare's equivalent of speaking fluent binary. When I later reviewed my emergency visit records, I noticed how the app had pre-authenticated my coverage using tokenized credentials before arrival. That invisible handshake between app and hospital EHR systems meant registration took 90 seconds instead of 90 minutes. For someone potentially mid-heart attack? That's not efficiency - that's engineering empathy.
But the real witchcraft happened post-crisis. At 4 AM, doped on nitroglycerin and facing a prescription for blood thinners, the app's medication tracker became my guardian angel. It cross-referenced my new Rx against existing supplements, flagging a dangerous interaction with my turmeric capsules. That feature isn't just helpful - it's running continuous background checks using FDA's drug interaction database. When it pinged me at dawn with Walgreens availability notification, I realized this wasn't an app. It was a healthcare guardian.
Recovery became a strange digital tango. The stress management module used biofeedback through my smartwatch - when my heart rate spiked during follow-up anxiety, it would launch guided breathing exercises synced to my cardiac rhythm. The "Health Journal" feature transformed passive recovery into active partnership, letting me log symptoms that generated predictive analytics for my cardiologist. Seeing my own EKG readings alongside lifestyle data made abstract medical advice concrete: that third espresso really did cause PVCs visible on the rhythm strip.
Yet for all its brilliance, the app has moments of heartbreaking stupidity. Attempting to use its "Virtual Visit" feature during a panic attack felt like negotiating with a brick wall. The AI triage bot kept looping: "Describe your symptoms. Are you experiencing chest pain?" YES YOU TONE-DEAF ALGORITHM - I TOLD YOU THREE TIMES! And don't get me started on the "health rewards" program that offered me a $2 Amazon coupon for nearly dying. This corporate gamification of survival left me equal parts furious and hysterical - like receiving a participation trophy from the reaper.
The Ghost in the Machine
What unsettles me most? How this app learns. After my cardiac scare, it began serving up eerily specific content - articles about young-onset heart disease exactly matching my demographics. When I mentioned Mediterranean diets to my therapist during a telehealth session accessed through the app, recipe suggestions appeared the next day. That whisper-thin line between helpful and invasive haunts me. The app's machine learning models clearly ingest everything - from my step count to how long I stare at cholesterol reports. This digital intimacy creates uncomfortable questions: who owns the anxiety patterns it detects in my biometrics? What happens when predictive analytics become pre-emptive interventions?
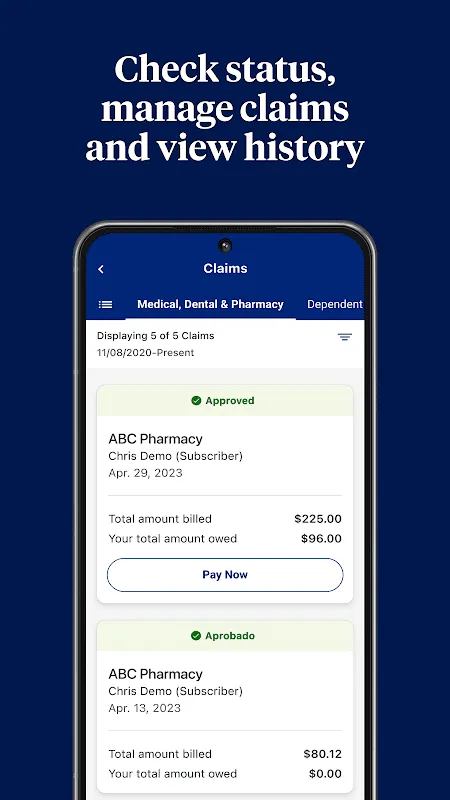
Still, I've developed a grudging dependency. The medication refill automation saved me when post-hospital brain fog made me forget my Plavix. The claim dispute feature fought a $3,800 air ambulance bill I was too exhausted to challenge. And when I hesitantly tapped the "mental health resources" section during a 3 AM anxiety spiral, it connected me to a crisis counselor faster than 911 ever could. There's brutal irony in owing your life to the very industry that nearly bankrupted you - but that cognitive dissonance pales when you're staring at your own mortality.
Now, six months later, I still open it compulsively - not for emergencies, but for reassurance. That glowing blue icon represents something profound: the terrifying fragility of human bodies and the extraordinary technology keeping them running. My late-night scrolling through health records isn't hypochondria - it's the modern equivalent of checking your sword's sharpness before battle. This app transformed from ignored nuisance to digital lifeline, embedding itself into my survival instincts until I reflexively reach for my phone before my own pulse during moments of fear.
Would I recommend it? With caveats that taste like ashes. Yes - if you enjoy corporate surveillance packaged as salvation. Absolutely - if you want healthcare's bureaucratic nightmare distilled into something resembling human compassion. The UnitedHealthcare app holds a mirror to American medicine's broken soul - simultaneously miraculous and mercenary. But when that next midnight terror grips my chest? You'll find me already logged in, watching that real-time ER wait countdown like a holy mantra. My cardiologist calls it PTSD. I call it pragmatism. The app just calls it Tuesday.
Keywords:UnitedHealthcare,news,cardiac emergency,healthcare technology,digital health management









