My Midnight Rescue with Unyte
My Midnight Rescue with Unyte
Rain lashed against my home office window when Sarah's alert pulsed through my tablet at 11:37 PM - that distinctive chime only triggered by critical distress signals. My fingers trembled slightly as I swiped open the neural platform, adrenaline cutting through exhaustion. There she was in split-screen view: left side showing her live heart rate spiking at 128 bpm, right side displaying the jagged EEG patterns screaming autonomic chaos. Her panicked voice crackled through the speaker: "It's happening again... the walls..."
I guided her shaking hands toward the biofeedback module, watching real-time coherence scores flicker between red and amber. "Match the wave, Sarah," I urged, demonstrating slow diaphragmatic breathing into my own sensor. The haptic pulse in her wristband synced with my rhythm - that brilliant tactile cue cutting through her dissociation. When her HRV graph finally steadied into green waves ten minutes later, tears pricked my eyes. This wasn't just therapy; it was intercepting a neurological emergency from three counties away while wearing pajamas.
What floored me wasn't merely the remote capability, but how The Science Beneath transformed interventions. During Sarah's stabilization, I accessed her historical baselines overlayed against current readings - seeing exactly how trauma had hijacked her default mode network. The platform's algorithms detected micro-shifts invisible to human observation: that 0.3-second delay in prefrontal response signaling dissociation onset. When I adjusted the neurostimulation frequency mid-session, I witnessed her amygdala reactivity dampen within seconds on the fMRI-mapped interface. This granularity turned guesswork into precision warfare against dysregulation.
Yet Tuesday's session revealed the platform's infuriating limitations. Midway through exposure therapy, Sarah's audiovisual feed froze during a critical window of tolerance. The session analytics later revealed what I'd missed: a 12-second latency spike where her galvanic skin response plummeted off the charts. "I felt abandoned when your face pixelated," she confessed during debrief. That technological betrayal undid weeks of trust-building - a harsh reminder that digital therapy tools remain hostage to bandwidth gods. The incident report I filed still sits unanswered in their support portal.
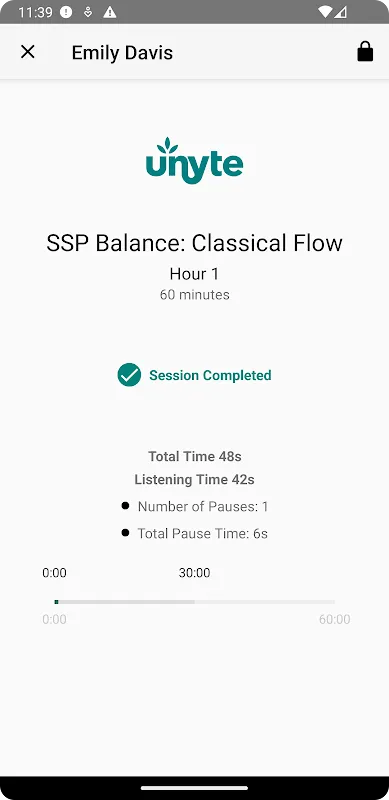
Post-midnight interventions became our strange ritual. Over six weeks, I watched Sarah's neural landscapes transform through cumulative data visualizations. The breakthrough came when we co-created her "neuro-signature" - a personalized stability protocol blending binaural beats with bilateral stimulation. The evening her coherence score held steady through triggering stimuli, we celebrated via screen-shared animated fireworks in the app. Her laughter echoing through my speakers carried more healing than any clinic session.
Now when crisis alerts ping after hours, I grab my tablet with battlefield intensity. The platform's cold metrics hold life-altering power - watching cortisol markers dip during virtual forest walks, or dopamine spikes when clients unlock achievement badges. But last full moon revealed new magic: Sarah guided me through breathing exercises when power outages trapped me during a storm. That role reversal, made possible by this shared neural language, shattered my clinician-client paradigm forever. This distributed healing ecosystem doesn't just extend therapy beyond walls; it rewires therapeutic relationships at molecular levels.
Keywords:Unyte Health,news,neural coherence,biofeedback therapy,remote intervention









