My Solo Trek Turned Medical Nightmare with Dialogue
My Solo Trek Turned Medical Nightmare with Dialogue
I’ve always prided myself on being prepared for anything—packed extra batteries, a first-aid kit, and even a satellite communicator for my week-long hiking trip through the Scottish Highlands. But nothing could have prepared me for the searing, gut-wrenching pain that exploded in my abdomen on the third day, miles from any road or village. As dusk settled and temperatures dropped, my bravado evaporated into sheer terror. Curled up in my tent, with only the howling wind for company, I felt utterly isolated, my mind racing through worst-case scenarios: appendicitis, infection, or something far worse. In that moment of primal fear, my phone’s glow felt like a feeble lifeline, until I remembered the health app I’d downloaded on a whim weeks earlier—a decision that would soon rewrite my story from potential tragedy to one of gritty survival.
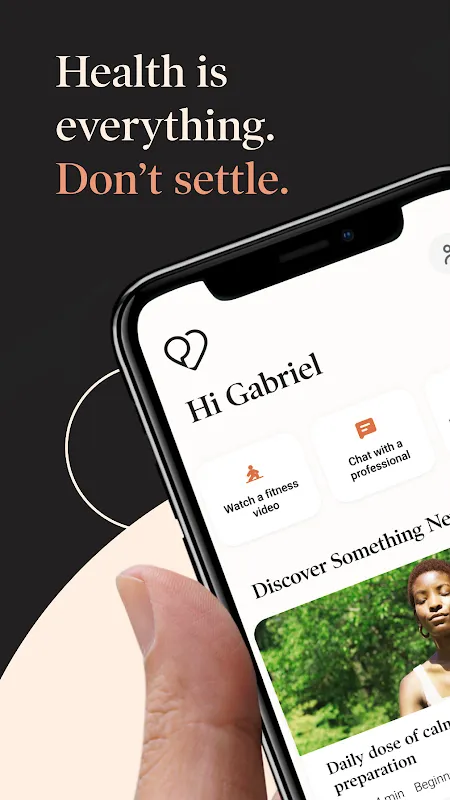
Fumbling with numb fingers, I launched the application, its interface loading with an almost eerie calmness against my panic. The design was minimalist—no flashy graphics, just clear options for immediate help. I tapped "Urgent Care," and within seconds, a connection was establishing. The video quality was astonishingly crisp despite my spotty cellular signal; later, I learned it uses adaptive bitrate streaming to prioritize stability over resolution in low-network areas. A face appeared—Dr. Aris, her expression professional yet reassuringly human. "I see you’re in distress. Can you describe your symptoms?" she asked, her voice cutting through the static like a warm blanket. I stammered out details about the pain’s location and intensity, while the app’s backend likely used AI triage algorithms to categorize my emergency level, though it felt seamlessly human.
As Dr. Aris guided me through self-assessment—pressing on specific areas, checking for fever—the app’s real-time symptom logging feature allowed her to note everything without breaking flow. She had me use my phone’s flashlight to show my tongue and abdomen, and the video compression tech minimized lag, making it feel like she was right there. "Based on what I’m seeing, it might be early appendicitis, but we need to rule out other issues," she said calmly, her tone never dipping into alarmism. She recommended I avoid moving drastically and arranged for a local rescue team via the app’s partnership with emergency services—a integration that uses GPS mapping to coordinate nearest responders. Waiting alone in the dark, I oscillated between gratitude and frustration; why hadn’t I invested in a personal locator beacon sooner? But the app’s efficiency was undeniable.
Thirty minutes later, help arrived—a testament to the geolocation precision embedded in the platform. As I was stretchered out, Dr. Aris stayed on video until handoff, her presence a digital anchor in the chaos. At the hospital, tests confirmed her suspicion: early-stage appendicitis, caught in time thanks to remote intervention. Recovery was swift, but the emotional aftershocks lingered. I became obsessed with dissecting how this tool worked—its encryption for patient data (end-to-end, I discovered), its network of certified professionals available 24/7, and even its mental health modules I explored post-recovery. Yet, it wasn’t flawless; during peak usage, I’d heard stories of slight delays, and the subscription cost made me wince—a stark reminder that cutting-edge care often comes with a price tag.
Now, back in the urban grind, I keep the app on my home screen—not as a crutch, but as a symbol of modern resilience. It’s transformed how I view healthcare: no longer a distant institution, but a tap away. The experience left me with a mix of awe and critique; while the technology is revolutionary, it’s not a substitute for systemic access issues. But in those Highland mists, it was nothing short of a lifeline.
Keywords: Dialogue,news,telemedicine,emergency response,remote wellness









