Night Shift Salvation with ParaPass
Night Shift Salvation with ParaPass
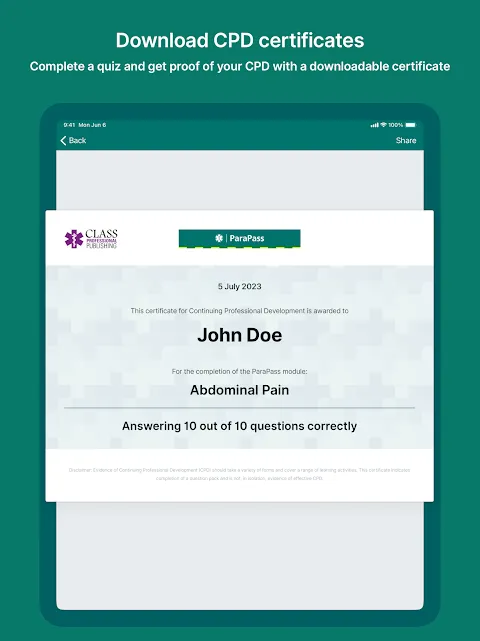
Rain lashed against the ambulance windows like gravel thrown by angry gods as I slumped against the gurney straps, the metallic tang of adrenaline still coating my tongue. My fingers trembled – not from the cardiac arrest call we'd just lost, but from the damning red notification on my phone: "CPD CERTIFICATION EXPIRED." Fourteen years on the job, and I was one bureaucratic oversight away from suspension. The roster showed five more night shifts this week, each a minefield of possible audits. Panic coiled around my ribs like a blood pressure cuff cranked too tight.
That's when Carlos slid his cracked phone across the stretcher. "Try this before you hyperventilate into a paper bag," he muttered, grease from the kebab he was eating smearing the screen. The app icon glowed – a blue shield with a lightning bolt. First tap: instant relief. Not some corporate LMS monstrosity demanding 40-hour modules, but bite-sized scenarios I could actually digest between overdoses and obstetric emergencies. The interface loaded before my finger left the glass, presenting a 3-minute pediatric sepsis drill based on last week's failed resuscitation. How did it know? Later I'd learn its algorithm tracked my response patterns like an ECG reading.
What followed wasn't learning – it was survival. During a lull at 3AM, parked behind a methadone clinic, I tackled airway management modules while chewing nicotine gum. The app didn't just show textbook diagrams; it made me feel the cricoid cartilage through haptic feedback synced to instructional videos. When I failed a difficult airway simulation, it didn't shame – it decomposed my errors in real-time. "Compression depth inconsistent during hypoxia phase," flashed the analysis, pinpointing exactly when my virtual hands shook. That adaptive machine learning engine became my brutal, brilliant drill sergeant.
Then came Thursday's disaster. Multi-vehicle pileup on the interstate, rain turning blood into pink slush on asphalt. A teenager trapped with bilateral femur fractures screamed as her BP plummeted. My mind blanked – until muscle memory from ParaPass kicked in. The app's trauma triage drills had rewired my instincts. I visualized the interactive hemorrhage control module as I packed the wound, hearing the app's calm prompt: "Tourniquet placement verified." Later, the ER doc raised an eyebrow at my textbook application. "ParaPass?" he asked, and I just nodded, too exhausted to explain how a stupid phone app had just saved two lives.
But Christ, the offline mode betrayed me during a rural transport. Middle of nowhere, zero signal, trying to access pediatric dosing charts as an infant seized in the back. The app stuttered, cached files corrupted, leaving me swearing at loading screens while calculating milligrams by penlight. That rage-fueled moment made me slam my fist against the oxygen tank – a dent I'd later explain as "equipment damage during emergency maneuvers."
Now it lives in my bunker gear pocket, its notification buzz more familiar than my pager. Sometimes I resent its relentless efficiency – the way it pushes neonatal resuscitation drills after I've delivered my third stillbirth of the month. Yet when I finally renewed my certification last week, I didn't feel pride. Just cold fury that this evidence-based lifeline isn't standard issue for every EMT. We gamble with lives daily while hospitals waste millions on glossy simulation labs collecting dust. ParaPass? It meets us in the blood-soaked trenches where real medicine happens.
Keywords:ParaPass,news,paramedic training,emergency medicine,CPD certification









