Recovery Rewired: An App Story
Recovery Rewired: An App Story
Rain lashed against the window as I fumbled with the pill bottle, my left arm strapped in a sling after rotator cuff surgery. The surgeon's discharge papers lay water-stained and illegible on the coffee table—I'd knocked over a glass in my morphine haze. Every twinge in my shoulder felt like a betrayal, whispering: You'll never lift your grandkids again. That’s when my phone buzzed—a text from the clinic: "Download Force Patient. Your care team is waiting." Skepticism curdled in my throat. Another app? Probably some corporate checkbox disguised as compassion.
Force Patient opened with a soft chime, no flashy animations—just a stark white interface and a video thumbnail of Dr. Evans. Tapping it, his familiar face filled the screen: "Mark, remember: ice pack intervals are critical today." His finger pointed precisely at a 3D model of my shoulder joint. No jargon, no PDFs lost in digital purgatory. Just him, in my living room, explaining scar tissue formation like we were sharing coffee. The relief was visceral—a warm wave unknotting the cold dread in my stomach. For the first time since surgery, I exhaled.
The Ghost in the Machine
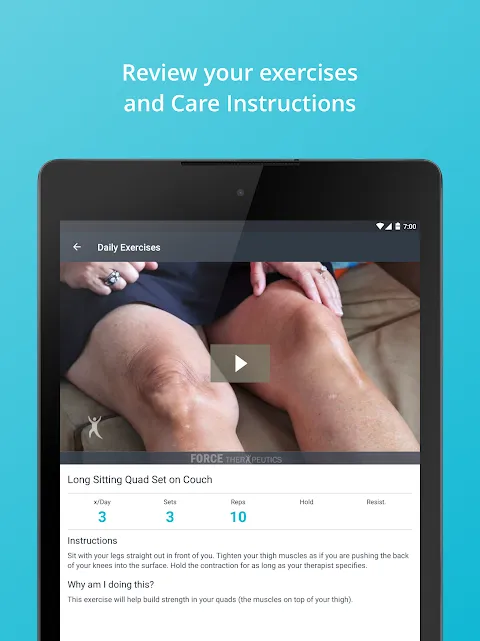
By day three, the app’s daily tasks became my scaffolding. "Gentle pendulum exercises NOW" flashed at 10 AM sharp. I’d procrastinated, dreading the pain, but Force Patient didn’t nag—it showed a 20-second loop of my physical therapist demonstrating the motion. Adaptive bitrate streaming meant zero buffering, even on my rural Wi-Fi. As I swayed my arm gingerly, the app logged each rep. Later, reviewing the data, I noticed a pattern: my range of motion improved most after icing. Obvious? Maybe. But seeing it graphed—blue lines inching upward—made me feel like a scientist decoding my own body. That’s when the addiction started. I’d catch myself checking progress charts instead of doomscrolling Twitter.
Midnight Panic and Pixel Lifelines
Then came the 2 AM terror. A searing heat bloomed around my incision—red, angry streaks radiating outward. Infection? Blood clot? My mind spiraled into ER wait times and medical bankruptcy. Hands shaking, I mashed the real-time support button. Within 90 seconds, Nurse Anya’s face pixelated onto my screen. "Show me," she commanded. I angled my phone, tears blurring the lens. She zoomed in—a feature using edge-computing to enhance image clarity without draining bandwidth. "Allergic reaction to the adhesive," she diagnosed, calm as a bomb defuser. "Take Benadryl. I’ve paused your morning meds." Her avatar blinked out, leaving silence and the hum of my refrigerator. No ambulance. No $500 co-pay. Just… solved.
But the app wasn’t flawless. One rainy Tuesday, it glitched during sync—my pain-log entries vanished. Rage spiked hot and sudden. I nearly hurled my phone against the wall. Why trust a cloud-based architecture with my vulnerability? Later, I’d learn it was an iOS update conflict, not Force Patient’s fault. Still, in that moment, betrayal bit deep. Tech fails shouldn’t feel like your lifeline snapping.
Weeks blurred. Force Patient’s milestones chimed like tiny victories: "First full rotation achieved!" I’d celebrate with single-arm air punches. The care team messaged encouragement between check-ins—"Your consistency is impressive, Mark"—making isolation feel like teamwork. By discharge day, deleting the app felt like parting with a battle buddy. My shoulder? Still stiff. But the fear? Disarmed. Force Patient didn’t heal me. It handed me the scalpel to carve my own recovery.
Keywords:Force Patient,news,surgery recovery,health tech,real-time care









