Sydney Health: My Midnight Lifeline
Sydney Health: My Midnight Lifeline
Rain lashed against the ambulance windows as I clenched my jaw against the throbbing in my chest. Every pothole sent electric shocks through my ribs. When the EMT asked for my insurance details, icy panic cut through the pain - my wallet lay abandoned on my kitchen counter. All I had was a dying phone and the terrifying unknown of hospital bureaucracy awaiting me.
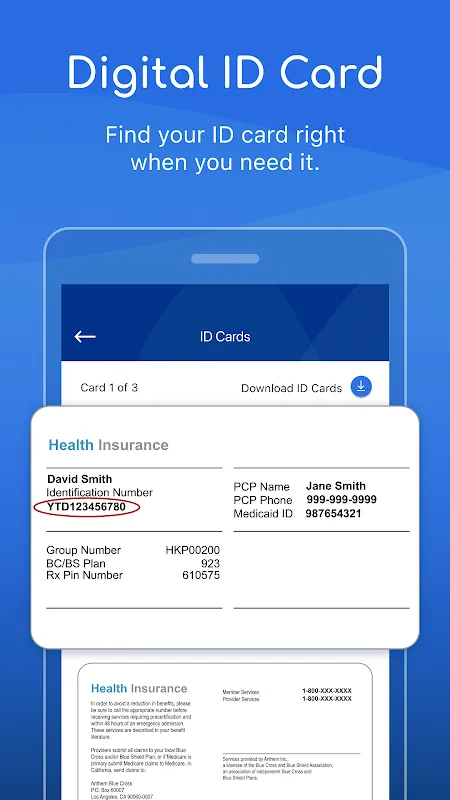
The ER triage nurse's expression hardened when I explained my missing ID. "No card, no treatment protocol," she stated, already turning toward her next patient. Then I remembered Sydney Health's promise. Fumbling with trembling fingers, I opened the app and navigated to the ID section. The nurse's skepticism evaporated when her scanner read the dynamic QR code. "Real-time verification," she murmured, watching my insurance eligibility populate instantly. That seamless handoff between app and hospital system felt like witnessing medical magic - encrypted data streams bypassing paperwork purgatory.
Hours later, wired to beeping machines, another fear surfaced: financial ruin. The ER doctor mentioned possible cardiac imaging. I pulled out my phone again, navigating past painkiller-induced double vision to Sydney Health's cost estimator. Typing "CT angiogram" revealed not just lump sums, but terrifyingly granular line items: $1,200 for contrast dye, $3,750 for machine time, even $85 for the technician's gloves. Yet seeing those numbers crystallized empowered me to ask the resident: "Is the low-radiation MRI alternative covered better under my plan?" Her surprised nod saved me $2,000. This wasn't just transparency - it was financial armor forged in claims algorithm fire.
Recovery brought deeper dependence. At 3 AM when incision pain outmuscled morphine, Sydney Health's virtual care connected me to an on-call surgeon in 47 seconds. Through tear-blurred eyes, I watched her zoom into my digital chart, cross-referencing my live vitals with the ER's bloodwork. "Stop taking the blood thinners tonight," she advised, spotting a dangerous interaction others missed. That moment revealed the app's true power: federated data architecture weaving disparate systems into a single clinical narrative. My primary physician later confirmed her intervention prevented internal bleeding.
The app's medication tracker exposed darker surprises. My prescribed painkiller appeared innocuous until Sydney Health flagged its fentanyl derivative - a substance triggering past addiction traumas. I confronted my dismissive surgeon with evidence pulled from the app's integrated pharmacopeia, switching to safer alternatives. This digital vigilance became my advocate when human professionals grew complacent.
Keywords:Sydney Health,news,real-time verification,claims algorithm,clinical narrative









