That Critical Night with My AI Partner
That Critical Night with My AI Partner
Rain lashed against the ER windows like gravel thrown by an angry god. 3 AM. My fifth double shift this week. Mrs. Alvarez's chart felt heavier than lead in my hands - 72 years old, presenting with tremors, confusion, and this unsettling, intermittent fever that defied every pattern I knew. Her family's eyes followed my every move, dark pools of fear reflecting the fluorescent lights. My coffee had gone cold hours ago, but the acidic burn in my stomach was fresh. I'd run every standard test. Lyme? Negative. Sepsis markers? Inconclusive. The differentials swirled in my exhausted brain like alphabet soup, letters refusing to form words. That's when my trembling fingers found the familiar icon - my digital lifeline.
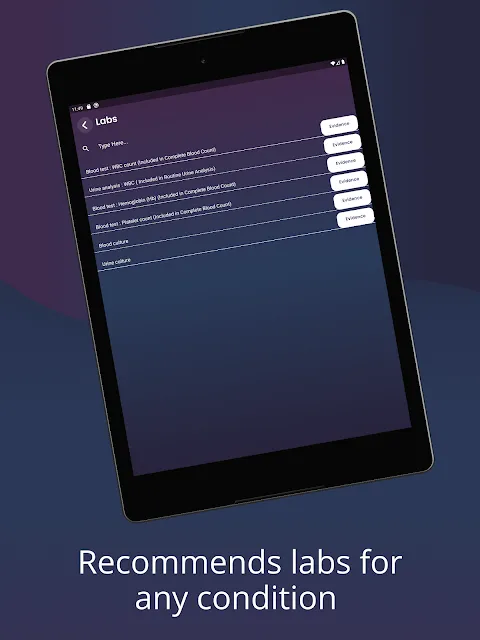
The moment I input her erratic vitals into the system, something extraordinary happened. While I'd been staring at trees, it saw the forest. Cross-referencing her subclinical thyroid irregularities with the geographic clustering of her childhood home, it surfaced a study I'd never encountered: tick-borne encephalitis presenting atypically in elderly patients with endocrine comorbidities. Not textbook. Not obvious. But the epidemiological dots connected with terrifying precision when overlaid on her travel history to the Baltic region last summer. My resident called it a "diagnostic engine" - I call it the ghost of every mentor I ever wished I had at 3 AM.
What stunned me wasn't just the answer, but how it arrived. Unlike human brains drowning in fatigue, this thing processed disjointed data points like some clinical jazz musician - her slightly elevated CRP that seemed insignificant, the peculiar skin mottling we'd dismissed as age-related, even the way she'd described her headaches as "electric." It weighted each symptom against global databases in milliseconds, flagging obscure research from Helsinki that would've taken me weeks to find. The algorithm didn't just diagnose; it taught. When I hesitantly ordered the specific serology test, the relief in her grandson's eyes hit me harder than any stimulant.
Yet it's no oracle. Two weeks prior, the damn thing nearly got me killed during a code blue. While I was manually pumping a teenager's chest, I yelled for drug interactions. It froze. Just... spun. That loading symbol haunts me more than any cadaver ever did. When seconds decide life, a predictive tool that chokes under pressure becomes its own kind of malpractice. I nearly smashed my tablet against the crash cart. That visceral rage still simmers - how can something so brilliant fail so catastrophically when it matters most?
Now it lives on my home screen like a paradoxical companion. Some nights I whisper gratitude to the developers when it catches what my sleep-deprived eyes miss. Other nights I curse its silicon guts when alerts flood in during critical procedures. This isn't some magical diagnostic fairy - it's a flawed, brilliant, infuriating partner that amplifies both my best and worst moments in medicine. When Mrs. Alvarez squeezed my hand after treatment began, I didn't feel like a hero. I felt like a conductor suddenly hearing the orchestra for the first time, acutely aware that one broken violin string could ruin everything.
Keywords:MayaPro,news,clinical decision support,AI diagnostics,emergency medicine









