When Seconds Counted, Data Saved Us
When Seconds Counted, Data Saved Us
The fluorescent lights of the emergency waiting room flickered like my frayed nerves. My husband clutched his chest, skin waxy and clammy, as triage nurses fired questions I couldn't answer. "Current medications? Dosage changes? Recent ECGs?" My mind blanked - the stress obliterating details I swore I knew. Then my thumb found the cracked screen of my phone. Opening the teal icon felt like throwing a life preserver into stormy seas.
Scrolling through ManageMyHealth NZ, I watched the nurse's eyes widen as I rattled off precise details: 80mg daily of blood thinner increased two weeks prior, the exact timestamp of his abnormal stress test, even the PDF of his implanted pacemaker's serial number. Her tablet synced with hospital systems while I spoke, pre-loading decades of cardiac history before we reached the cath lab doors. The ER physician later told me those fifteen minutes of comprehensive data shaved critical time off his treatment window.
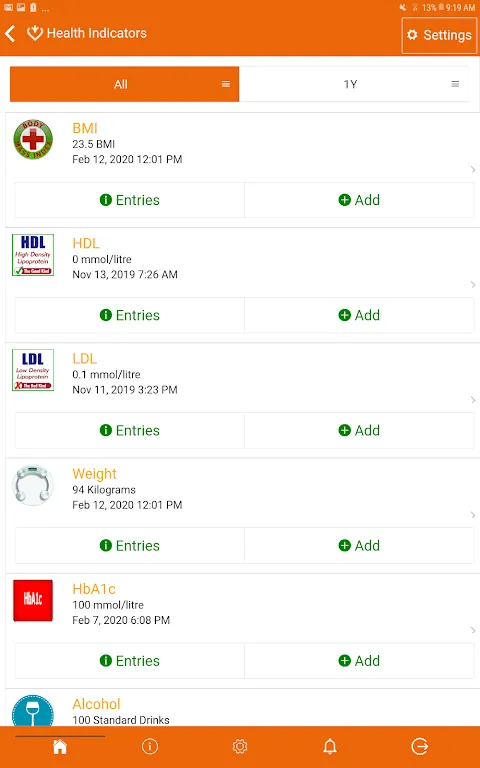
This wasn't passive record storage. The platform's architecture revealed itself in that crisis. When I uploaded his cardiologist's handwritten notes last month, optical character recognition transformed doctor-scrawl into searchable text. Integration protocols pulled fresh lab results directly from diagnostic centers - no more playing telephone tag with receptionists. Yet the true genius lived in the timeline view: color-coded markers plotting cholesterol spikes against medication changes, creating visual narratives where paper files offered only fragments.
Flaws surfaced brutally in recovery. That elegant medication tracker? Useless when his new prescription didn't auto-populate for 72 hours because some clinic fax machine still thought it was 2003. I nearly overdosed him on discontinued pills, saved only by physical packet cross-checking. And don't get me started on the "urgent alert" feature - notifications about critical updates buried beneath supermarket coupons like medical priorities playing hide-and-seek.
Yet when specialists debated stent options during rounds, I became an unexpected authority. Pulling up angiograms side-by-side with bloodwork trends on my tablet revealed patterns even residents missed. "How are you accessing this?" asked the lead cardiologist, peering at real-time medication interaction flags I'd triggered. That moment flipped our dynamic - from helpless family member to informed collaborator armed with data.
Security anxieties linger though. Each biometric login feels like gambling with his most intimate secrets. The app boasts military-grade encryption, but I've seen health platforms crumble under breaches. Still, the alternative terrifies me more: that nightmarish ER experience multiplied across every future emergency. So I compromise - disabling location permissions, using burner emails for login, treating each sync like handling radioactive material.
Now, hospital discharge papers get scanned before we leave parking garages. I harass pharmacists until they push digital scripts directly into the system. This health management beast demands constant feeding, but the payoff crystallized last week: his new GP reviewed seven years of coordinated data in twelve minutes flat. No faxes. No lost files. Just the quiet hum of interoperability finally working as intended.
Keywords:ManageMyHealth NZ,news,emergency care,health data integration,medical interoperability









