decision support 2025-10-30T00:23:30Z
-
 ScreenMeet Support*ONLY DOWNLOAD IF DIRECTED TO DO SO BY A SUPPORT TECHNICIAN YOU TRUST*Screen Meet Support allows support technicians to troubleshoot a problem you are having on your Android device. To use this application you must be receiving support from a technician who is using ScreenMeet Support and will provide you a Session code to start the session.Technicians have the ability to see your screen and to use a laser pointer to indicate where you should tap. You can show them your Android
ScreenMeet Support*ONLY DOWNLOAD IF DIRECTED TO DO SO BY A SUPPORT TECHNICIAN YOU TRUST*Screen Meet Support allows support technicians to troubleshoot a problem you are having on your Android device. To use this application you must be receiving support from a technician who is using ScreenMeet Support and will provide you a Session code to start the session.Technicians have the ability to see your screen and to use a laser pointer to indicate where you should tap. You can show them your Android -
 Decision RouletteYou have to make a decision and don't know what to choose?Sometimes it is better to leave it all to fate!The Decision Roulette helps you to choose among the various options available. You can write from 2 to 50 options in different roulettes and use them whenever you want. You can also add images to each option. The images must be png/jpg and must be stored in your device. The information is only saved on the device, not in the cloud.It is free, easy to use and you can find it u
Decision RouletteYou have to make a decision and don't know what to choose?Sometimes it is better to leave it all to fate!The Decision Roulette helps you to choose among the various options available. You can write from 2 to 50 options in different roulettes and use them whenever you want. You can also add images to each option. The images must be png/jpg and must be stored in your device. The information is only saved on the device, not in the cloud.It is free, easy to use and you can find it u -
 Knox Remote SupportKnox Remote Support is a remote troubleshoot solution which allows IT admins to remotely connect to the user's device of Knox cloud services.Knox Remote Support provides: - Remotely control the user's device - Record device screen as a video clip and send to IT admin. - Capture device screen as an image file and send to IT admin. - Enables IT admin to send the files to the user and vice versa.Knox Remote Support is provided as a part of Knox cloud services on a valid license.
Knox Remote SupportKnox Remote Support is a remote troubleshoot solution which allows IT admins to remotely connect to the user's device of Knox cloud services.Knox Remote Support provides: - Remotely control the user's device - Record device screen as a video clip and send to IT admin. - Capture device screen as an image file and send to IT admin. - Enables IT admin to send the files to the user and vice versa.Knox Remote Support is provided as a part of Knox cloud services on a valid license. -
 Remote Support ezHelpezHelp is remote support application for customer.[Feature]- Multi OS supportWindows PC, Apple OS, Android-Fast and Powerful remote controlFast and powerful remote control by hardware driver technology.-Various network support (Private IP, Firewall, VPN, etc)You can remote control without network settings.-Remote soundYou can listening remote pc's sound during remote control.-Network access optimizeFast remote control through access algorithm optimize. -MS OS optimizeWindows
Remote Support ezHelpezHelp is remote support application for customer.[Feature]- Multi OS supportWindows PC, Apple OS, Android-Fast and Powerful remote controlFast and powerful remote control by hardware driver technology.-Various network support (Private IP, Firewall, VPN, etc)You can remote control without network settings.-Remote soundYou can listening remote pc's sound during remote control.-Network access optimizeFast remote control through access algorithm optimize. -MS OS optimizeWindows -
 Child Support SpecialistsChild Support Specialists is the oldest private child support agency in Texas. We are licensed and bonded. We normally can collect in 30 - 60 days. We work court order and non-court order child support cases. We provide advanced locate information on all cases. We also provide paternity testing with or without a child support case. Apply now by clicking the application button. 800-380-5437281-277-5437http://www.csskids.com
Child Support SpecialistsChild Support Specialists is the oldest private child support agency in Texas. We are licensed and bonded. We normally can collect in 30 - 60 days. We work court order and non-court order child support cases. We provide advanced locate information on all cases. We also provide paternity testing with or without a child support case. Apply now by clicking the application button. 800-380-5437281-277-5437http://www.csskids.com -
 Google Support ServicesThe Google Support Services (GSS) app allows you to share your Android device screen with a Google customer support agent for a personalised support experience. With GSS on your device, the agent can invite you to share your screen and guide you with on-screen annotations, making it faster and easier to resolve your issue. While sharing your screen, the agent will not be able to control your device, but will be able see your screen to help explain their instructions. You c
Google Support ServicesThe Google Support Services (GSS) app allows you to share your Android device screen with a Google customer support agent for a personalised support experience. With GSS on your device, the agent can invite you to share your screen and guide you with on-screen annotations, making it faster and easier to resolve your issue. While sharing your screen, the agent will not be able to control your device, but will be able see your screen to help explain their instructions. You c -
 Daybreak - Alcohol SupportDaybreak helps you change your relationship with alcohol. Whether your goal is to reduce your drinking, or complete abstinence, Daybreak is here to support you and your choice. Changing behaviour around alcohol use can be challenging, but you don't have to do it alone. Daybreak is a supportive and non-judgemental space where you can get the information and support you need to help achieve your goal. People who use Daybreak say they love waking up without hangovers, feel
Daybreak - Alcohol SupportDaybreak helps you change your relationship with alcohol. Whether your goal is to reduce your drinking, or complete abstinence, Daybreak is here to support you and your choice. Changing behaviour around alcohol use can be challenging, but you don't have to do it alone. Daybreak is a supportive and non-judgemental space where you can get the information and support you need to help achieve your goal. People who use Daybreak say they love waking up without hangovers, feel -
 ianacare - Caregiving Supportianacare is an integrated platform for family caregivers that organizes and mobilizes all the layers of support. Coordinate help with friends & family, utilize employer benefits, discover local resources, and get personalized guidance from our Caregiver Navigators.* Our mission is to encourage, empower and equip family caregivers with the tools and communities, so no caregiver does it alone.The first layer of support is rallying personal social circles (friends, fami
ianacare - Caregiving Supportianacare is an integrated platform for family caregivers that organizes and mobilizes all the layers of support. Coordinate help with friends & family, utilize employer benefits, discover local resources, and get personalized guidance from our Caregiver Navigators.* Our mission is to encourage, empower and equip family caregivers with the tools and communities, so no caregiver does it alone.The first layer of support is rallying personal social circles (friends, fami -
 Industry Online SupportIndustry Online Support is an application designed to provide users with access to a vast resource of information related to Siemens Industry products. It caters to professionals in various fields, allowing them to download the app for Android devices and utilize its extensive
Industry Online SupportIndustry Online Support is an application designed to provide users with access to a vast resource of information related to Siemens Industry products. It caters to professionals in various fields, allowing them to download the app for Android devices and utilize its extensive -
 DecidApp Demo. Decision MakingMake Better Decisions with Ease \xe2\x80\x93 Discover DecidApp, the ultimate decision-making app designed to empower you to make faster, better decisions with less stress. Whether you're deciding on personal matters or critical business choices, harness the power of decision trees to navigate complex choices confidently.Streamlined Decision Making \xe2\x80\x93 Create decision trees effortlessly with DecidApp's intuitive interface. Visualize information, update calcu
DecidApp Demo. Decision MakingMake Better Decisions with Ease \xe2\x80\x93 Discover DecidApp, the ultimate decision-making app designed to empower you to make faster, better decisions with less stress. Whether you're deciding on personal matters or critical business choices, harness the power of decision trees to navigate complex choices confidently.Streamlined Decision Making \xe2\x80\x93 Create decision trees effortlessly with DecidApp's intuitive interface. Visualize information, update calcu -
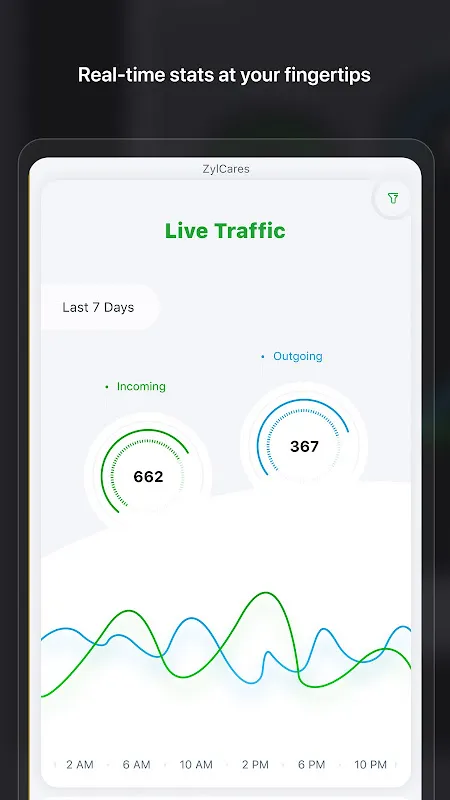 My knuckles turned white gripping the edge of my desk as the notification chimes became a continuous symphony of dread. Another holiday sale launch, another tidal wave of customer panic flooding our queues. I watched my team's Slack statuses blink from "available" to "in a call" like dying fireflies, knowing we were drowning in real-time. That's when I remembered the dashboard widget I'd half-heartedly installed weeks ago.
My knuckles turned white gripping the edge of my desk as the notification chimes became a continuous symphony of dread. Another holiday sale launch, another tidal wave of customer panic flooding our queues. I watched my team's Slack statuses blink from "available" to "in a call" like dying fireflies, knowing we were drowning in real-time. That's when I remembered the dashboard widget I'd half-heartedly installed weeks ago. -
 AWorld in support of ActNowAWorld is more than just an app\xe2\x80\x94it\xe2\x80\x99s a space where every action counts toward saving the Planet.Join the AWorld Community: the app for anyone who wants to live sustainably, take action against climate change, and improve their lifestyle.\xf0\x9f\x93\x8a Track and improve your lifestyleMeasure and reduce your impact with AWorld\xe2\x80\x99s Carbon Footprint tool. We provide practical tips to help you adopt a greener, more sustainable way of living.
AWorld in support of ActNowAWorld is more than just an app\xe2\x80\x94it\xe2\x80\x99s a space where every action counts toward saving the Planet.Join the AWorld Community: the app for anyone who wants to live sustainably, take action against climate change, and improve their lifestyle.\xf0\x9f\x93\x8a Track and improve your lifestyleMeasure and reduce your impact with AWorld\xe2\x80\x99s Carbon Footprint tool. We provide practical tips to help you adopt a greener, more sustainable way of living. -
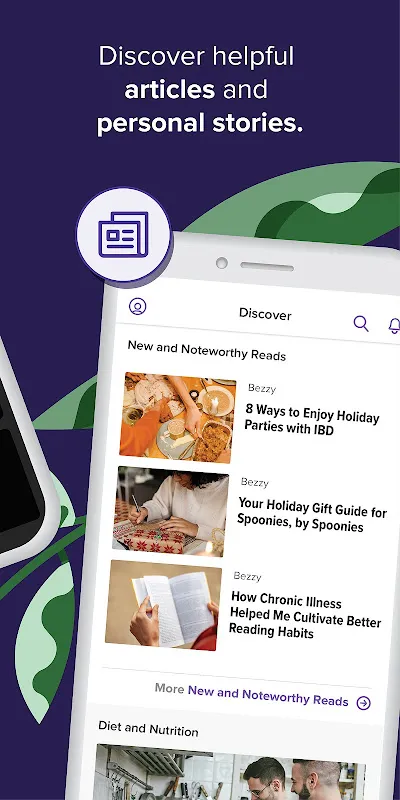 My hands shook holding the wedding invitation – a beach ceremony in Santorini. For two years, my ulcerative colitis had imprisoned me within a 20-mile radius of my gastroenterologist. The thought of navigating airports, foreign bathrooms, and unfamiliar food ignited a familiar dread. I traced the Mediterranean coastline on the invitation, imagining humiliating dashes through crowded alleys. That night, I lay awake obsessing over worst-case scenarios until sunrise painted my ceiling orange. Cance
My hands shook holding the wedding invitation – a beach ceremony in Santorini. For two years, my ulcerative colitis had imprisoned me within a 20-mile radius of my gastroenterologist. The thought of navigating airports, foreign bathrooms, and unfamiliar food ignited a familiar dread. I traced the Mediterranean coastline on the invitation, imagining humiliating dashes through crowded alleys. That night, I lay awake obsessing over worst-case scenarios until sunrise painted my ceiling orange. Cance -
 Hi-PrecisionHi-Precision Diagnostics App lets you access everything about your laboratory information for free.Monitor and download your online results and get updated with the latest news, promos, events and a lot more while you are on the go. Features:-Access Cumulative Results Online-Download Onl
Hi-PrecisionHi-Precision Diagnostics App lets you access everything about your laboratory information for free.Monitor and download your online results and get updated with the latest news, promos, events and a lot more while you are on the go. Features:-Access Cumulative Results Online-Download Onl -
 Venstar SkyportThe Venstar Skyport App allows Android users to remotely monitor and control their heating and cooling systems. From the couch to across town you have the ability to control your comfort remotely.Venstar Skyport App features include:\xe2\x9c\x94 Simple, easy to use monitor and control of the thermostat\xe2\x9c\x94 Current weather and forecast is displayed for each location\xe2\x9c\x94 Monitor equipment runtimes\xe2\x9c\x94 Receive thermostat alerts\xe2\x9c\x94 Easy selection of ho
Venstar SkyportThe Venstar Skyport App allows Android users to remotely monitor and control their heating and cooling systems. From the couch to across town you have the ability to control your comfort remotely.Venstar Skyport App features include:\xe2\x9c\x94 Simple, easy to use monitor and control of the thermostat\xe2\x9c\x94 Current weather and forecast is displayed for each location\xe2\x9c\x94 Monitor equipment runtimes\xe2\x9c\x94 Receive thermostat alerts\xe2\x9c\x94 Easy selection of ho -
 Dungeons and Decisions RPG\xf0\x9f\x8e\xb2Classic Roleplaying Simplified\xf0\x9f\x8e\xb2This is a series of fantasy novels where you get to make the choices for the main character. It is like a solo Dungeons & Dragons campaign, but far simplified. If you enjoy DnD tabletop games or fantasy novels li
Dungeons and Decisions RPG\xf0\x9f\x8e\xb2Classic Roleplaying Simplified\xf0\x9f\x8e\xb2This is a series of fantasy novels where you get to make the choices for the main character. It is like a solo Dungeons & Dragons campaign, but far simplified. If you enjoy DnD tabletop games or fantasy novels li -
 SUPPART - AI Art CreationWin a share of \xc2\xa5500,000 JPY in official contests! Earn points daily and redeem prizes like iPhones or Switch. Join the community to share ideas & stay updated.SUPPART \xe2\x80\x94 Create with a Tap, Unleash Your ImaginationEnter a keyword, choose a style, and our powerful AI will instantly generate unique images.With a simple and intuitive interface, anyone can create stunning artwork in seconds.\t\xe2\x80\xa2\tGenerate high-quality images for free\t\xe2\x80\xa2\t
SUPPART - AI Art CreationWin a share of \xc2\xa5500,000 JPY in official contests! Earn points daily and redeem prizes like iPhones or Switch. Join the community to share ideas & stay updated.SUPPART \xe2\x80\x94 Create with a Tap, Unleash Your ImaginationEnter a keyword, choose a style, and our powerful AI will instantly generate unique images.With a simple and intuitive interface, anyone can create stunning artwork in seconds.\t\xe2\x80\xa2\tGenerate high-quality images for free\t\xe2\x80\xa2\t -
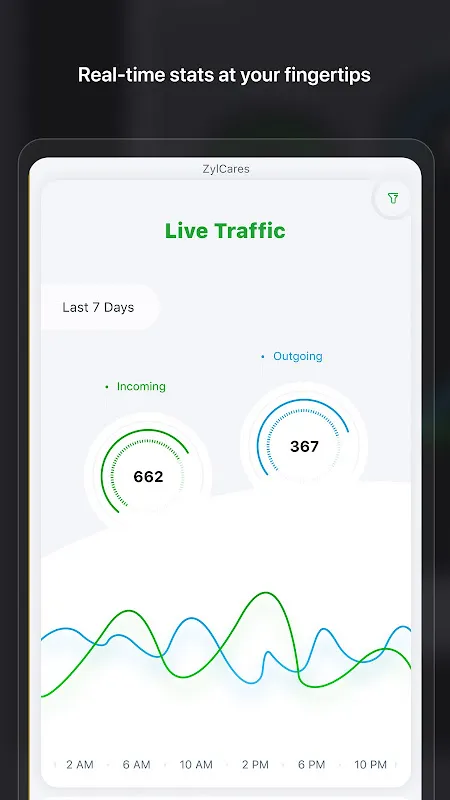 It was the Monday from hell. The holiday rush had hit our customer support team like a tidal wave, and I was drowning in a sea of unanswered tickets. My inbox was a bloated monster, each new email notification adding to the growing sense of panic. I could feel the tension in my shoulders, a tight knot that had been building since 6 AM, and the bitter taste of cold coffee lingered in my mouth as I frantically tried to prioritize issues based on gut feeling alone. We were flying blind, and I knew
It was the Monday from hell. The holiday rush had hit our customer support team like a tidal wave, and I was drowning in a sea of unanswered tickets. My inbox was a bloated monster, each new email notification adding to the growing sense of panic. I could feel the tension in my shoulders, a tight knot that had been building since 6 AM, and the bitter taste of cold coffee lingered in my mouth as I frantically tried to prioritize issues based on gut feeling alone. We were flying blind, and I knew

